As a BetterHelp affiliate, we receive compensation from BetterHelp if you purchase products or services through the links provided
Borderline Personality Disorder (BPD) is characterized by intense emotions, tumultuous relationships, and a pervasive fear of abandonment. At times, individuals with BPD may exhibit self-destructive behaviors, which can be both a cry for help and a coping mechanism for deep-seated pain. You need to understand that these actions are not indicative of personal failure but rather symptoms of a complex and often misunderstood personality disorder.
Self-destructive behaviors in the context of BPD may range from substance abuse to self-harm, risking personal safety, or sabotaging success. These actions often respond to overwhelming emotions that seem impossible to regulate. Emotions can be like a rollercoaster for someone with BPD, and self-destructive acts are sometimes used in an attempt to regain control or to express internal turmoil. It’s a painful paradox where the attempt to find relief can lead to further distress.
A holistic approach to treatment is crucial for individuals with self-destructive BPD. Therapy options like Dialectical Behavior Therapy (DBT) help teach emotional regulation and interpersonal effectiveness. A robust support system and a trusting therapeutic relationship can lay the foundation for recovery. It’s a journey that requires patience, understanding, and persistence, but with the right help, one can navigate a more stable and fulfilling life.
Key Takeaways
- Self-destructive behaviors in BPD are symptomatic responses to emotional pain and not personal failings.
- Emotional regulation and relationship challenges are central to understanding self-destructive BPD.
- Effective treatment involves a combination of therapy, support systems, and long-term management strategies.
 Understanding Borderline Personality Disorder
Understanding Borderline Personality Disorder
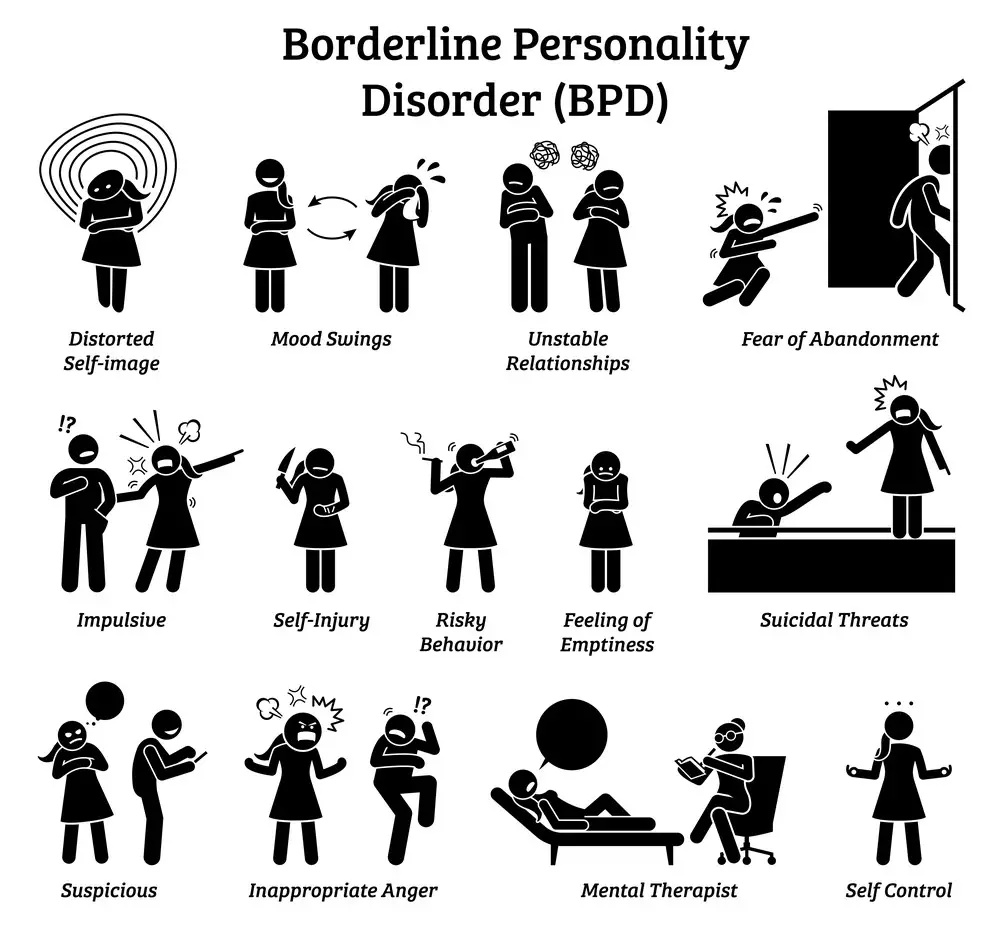
Borderline Personality Disorder (BPD) is a complex mental health condition marked by emotional instability, difficulties in interpersonal relationships, and a distorted self-image. It’s vital for you to recognize the signs and understand the nuances of this disorder to support those affected by it.
Core Characteristics of BPD
BPD is characterized by:
- Intense Emotional Swings: Your moods can change rapidly, which can be quite distressing.
- Fear of Abandonment: you might go to extreme lengths to avoid real or imagined separation or rejection.
- Unstable Relationships: Relations may fluctuate between idealization and devaluation.
- Unclear or Fluctuating Self-Image: A persistently unstable sense of self is common.
- Impulsive Behaviors: This might include spending sprees, unsafe sex, substance abuse, reckless driving, and binge eating.
- Self-Harm: Suicidal behavior and self-harm may occur as a response to fear of abandonment or rejection.
- Extreme Emotional Reactions: Stressful events can lead to panic, depression, or anger that’s difficult to control.
- Feelings of Emptiness: A sensation of void or boredom often troubles you.
- Difficulty Trusting: Paranoia or loss of contact with reality may manifest, usually under stress.
Key Takeaway: Understanding these core characteristics can help you empathize with the challenges faced by someone living with BPD.
Subtypes of BPD
The prominent psychologist Theodore Millon identified four BPD subtypes, each with distinct traits:
- Discouraged Borderline: Often feels helpless, dependent, and submissive. They may experience frequent feelings of dejection and at times, engage in self-harm.
- Impulsive Borderline: Characterized by thrill-seeking and risk-taking behaviors, people with this subtype may also exhibit charismatic and energetic behavior.
- Petulant Borderline: Unpredictable, irritable, and prone to feelings of unworthiness and fear of abandonment but also displays passive-aggressive behaviors.
- Self-Destructive Borderline: Engages in self-harm and has a pervasive sense of bitterness and self-deprecation.
Each subtype illustrates different manifestations of BPD symptoms, influencing how you might experience and respond to the disorder.
Key Takeaway: Recognizing the subtypes of BPD can guide you toward more tailored and effective strategies for managing the disorder.
 Causes and Contributing Factors
Causes and Contributing Factors
Understanding self-destructive behavior in Borderline Personality Disorder (BPD) is crucial for effective treatment. Let’s unpack the causes and see how they may be influencing behavior.
Role of Genetics and Environment
Genetics and your environment each contribute to the development of BPD. Here’s what you should keep in mind:
- Genetics: Studies show that BPD might run in families, which suggests a genetic predisposition. You might not inherit BPD directly, but you could inherit certain personality traits or emotional patterns.
- Environment: Your surroundings and life experiences, especially during childhood, play a significant role. A stressful or unstable environment can make you more prone to developing BPD.Key Takeaway: It’s a mix of inherited traits and your early environment that increases the risk of BPD.
Traumatic Events and Early Relationships
Trauma, particularly in your formative years, leaves a deep imprint on your emotional well-being. How you connect with family members and others can shape your view of relationships later in life.
- Traumatic Events: Experiencing traumatic events such as abuse or neglect can set you up for struggles with trust and self-worth.
- Early Relationships: Strong family relationships are a buffer against stress, but turbulent or absent bonds may lead to challenges in forming healthy relationships.Key Takeaway: Personal history plays a big part. Trauma may predispose you to BPD, and rocky early relationships often complicate matters further.
 Manifestations of Self-Destructive Behavior
Manifestations of Self-Destructive Behavior
Self-destructive behavior in the context of Borderline Personality Disorder (BPD) can be complex and varies from person to person. The following subsections provide a closer look at how these behaviors often present themselves.
Self-Harm and Suicidal Behavior
You might find individuals with BPD engaging in self-harm as a coping mechanism to manage overwhelming emotions or to break through feelings of numbness. Self-harm includes:
- Cutting or scratching the skin
- Burning the skin
- Hitting oneself or banging body parts against hard surfaces
Suicidal behavior is an extreme form of self-destructive behavior that may include:
- Suicidal thoughts: Persistent thoughts about wanting to end one’s life
- Suicidal threats: Making statements or warnings about taking one’s own life
- Suicide attempts: Engaging in behaviors with the intent to end one’s life
Key Takeaway: When feeling intense emotional pain, some individuals may turn to self-harm or experience suicidal tendencies as a form of expression or relief. It’s crucial to seek professional help if these behaviors are present.
Impulsivity and Reckless Behavior
Impulsivity in BPD manifests as spontaneous decisions without consideration of the consequences, such as:
- Spending sprees: Excessive or unnecessary shopping to alleviate distress
- Substance abuse: Using drugs or alcohol to dull or escape reality
- Reckless driving: Operating a vehicle in a dangerous manner
Reckless behavior might include engaging in risky sexual practices or other actions that jeopardize one’s safety. These behaviors are often a reaction to stress or emotional pain.
Key Takeaway: Impulsive and reckless actions can respond to internal turmoil; they may seem like quick fixes but can lead to more complex issues. Understanding your triggers can be a step toward managing these impulses.
 Emotional Dysregulation and Interpersonal Relationships
Emotional Dysregulation and Interpersonal Relationships
In self-destructive Borderline Personality Disorder (BPD), your relationships can often be complex and tumultuous, mainly because of emotional dysregulation, fear of abandonment, and attachment issues.
Challenges in Personal Relationships
Your experience with BPD might mean that feelings come on strong and fluctuate unpredictably. Emotional swings can be intense and fast, which can be bewildering not only for you but also for those close to you.
- Impulsive Reactions: Sometimes, without warning, you might react emotionally in ways that seem disproportionate to the situation.
- Difficulty Communicating: Expressing your feelings might present a real challenge, leading to misunderstandings and conflicts in relationships.
Having BPD can make maintaining stable, healthy relationships tough. You may notice a pattern where your relationships start intensely but then quickly become strained or may end abruptly.
Key Takeaway: Navigating personal relationships with BPD involves recognizing the fast-paced emotional changes and working towards better communication.
Fear of Abandonment and Attachment Issues
With BPD, a deep fear of abandonment often lurks in your relationships. It can cause you to misunderstand or misinterpret others’ actions as signs they’ll leave.
- Clingy Behavior: This fear might lead you to hold on too tightly to someone you love, which can, unfortunately, push them away.
- Attachment Style: You might notice your attachment to loved ones can be categorized as ‘anxious’ or ‘unstable’, meaning you’re often seeking reassurance of their love.
Understanding your attachment style can be a crucial step in understanding how you relate to others and working on forming more secure, less chaotic bonds.
Key Takeaway: Acknowledging and addressing your fears of abandonment can help you foster healthier and more secure attachments in your relationships.
Comorbidities and Differential Diagnosis
Navigating the complexities of Borderline Personality Disorder (BPD) often involves understanding its relationship with other mental health conditions. This can impact both treatment approaches and the accuracy of diagnosis.
Depression, Anxiety, and Other Disorders
BPD commonly coexists with mental health disorders such as depression and anxiety. These conditions can intertwine, creating a challenging cycle that may exacerbate self-destructive behaviors. It’s not unusual for you to experience:
- Persistent feelings of sadness or emptiness, indicative of depression
- Excessive worry about everyday events, which is a hallmark of anxiety
Key Takeaway: It’s essential to treat these comorbid conditions alongside BPD to improve overall well-being.
 Distinguishing BPD from Similar Conditions
Distinguishing BPD from Similar Conditions
When it comes to differentiating BPD from other conditions, particularly other personality disorders, the task can be quite intricate. For example:
- Bipolar Disorder: Characterized by dramatic shifts in mood and energy, bipolar disorder can sometimes be confused with BPD. However, mood swings in BPD are often triggered by interpersonal stressors and are more persistent compared to the episodic changes seen in bipolar disorder.
- Personality Disorders: While there are overlapping symptoms with other personality disorders, BPD is unique in its intense fear of abandonment and unstable interpersonal relationships.
Key Takeaway: Accurate diagnosis is critical and often requires a thorough evaluation by a mental health professional who can distinguish the nuances of these conditions.
Treatment and Therapy Options
When you’re facing the challenge of self-destructive behaviors in borderline personality disorder (BPD), it’s reassuring to know that there are specific treatment options designed to help you manage your emotions and reactions. These treatments are built on understanding and skill development to improve your quality of life.
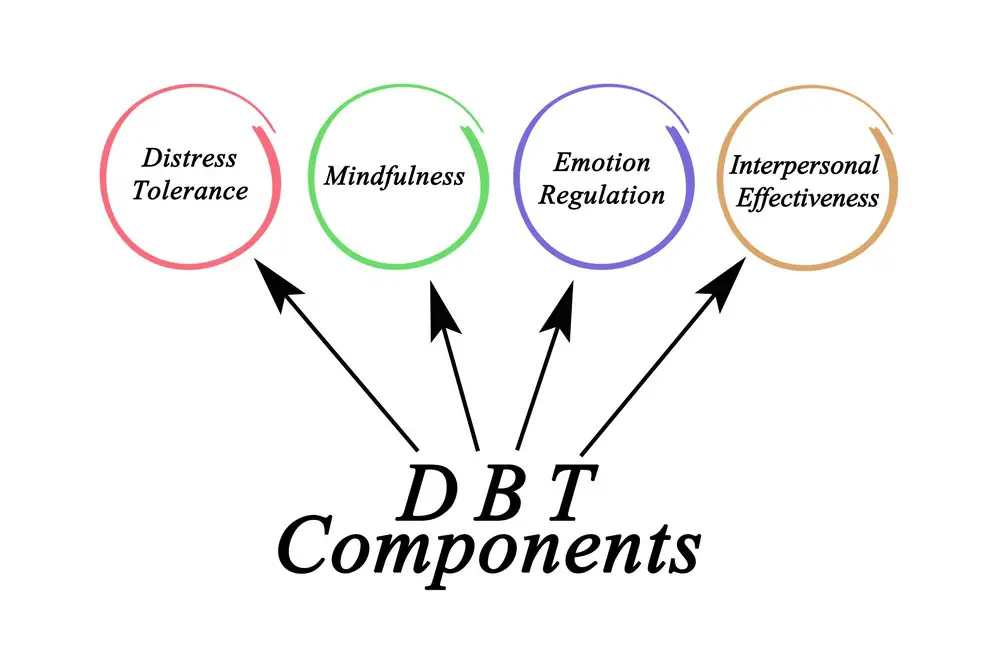
Dialectical Behavior Therapy (DBT)
Dialectical Behavior Therapy is a form of therapy tailored specifically for individuals with BPD. Its main goals are to:
- Teach mindfulness: which is being aware of the present moment without judgment.
- Increase distress tolerance: so you’re better equipped to handle tough situations.
- Enhance emotion regulation: to help you manage intense feelings.
- Improve interpersonal effectiveness: which means honing your communication and relationship skills.
DBT involves individual therapy sessions and group skills training classes, which typically occur once a week. In individual therapy, you’ll work one-on-one with a therapist to reflect on your progress and to tackle personal challenges. Meanwhile, group sessions offer a safe space to practice new skills with others who understand what you’re going through.
Key takeaway: DBT is a comprehensive approach that includes individual and group work, focusing on practical skills to reduce self-destructive behaviors.
Medications and Integrated Approaches
While there is no specific medication to cure BPD, certain medications can be prescribed to alleviate co-occurring symptoms, such as:
- Mood swings
- Depression
- Anxiety
These might include:
- Antidepressants (SSRIs, SNRIs)
- Mood stabilizers
- Antipsychotic medications
Yet, medications often work best when integrated with therapy. A multi-faceted approach can offer a more robust support system. By combining medication management with therapies like DBT, you create a personalized treatment plan that addresses various aspects of BPD. Always consult with a healthcare professional before starting or changing any medication regimen.
Key takeaway: Combining medication to mitigate symptoms and therapy to develop coping skills can enhance your treatment outcome.
Therapeutic Relationship and Recovery
In managing self-destructive behaviors associated with borderline personality disorder (BPD), the bond between you and your therapist is fundamental. It can pave the way to a more hopeful outlook and stronger coping mechanisms.
Importance of the Therapist-Patient Relationship
Trust and understanding: It’s crucial for you to feel understood and validated. A compassionate and nonjudgmental therapist helps foster a secure environment where you can be open about your struggles.
- Essential for engagement: Your commitment to therapy often hinges on how connected you feel with your therapist.
- Key to progress: A robust therapeutic relationship can lead to more significant strides in managing BPD symptoms.
Takeaway: A good therapist-patient relationship is the bedrock of effective therapy.
Building Hope and Coping Skills
Your journey is not just about managing symptoms; it’s about building a future that feels bright and attainable.
Hope: With guidance, you start to see beyond your current struggles and envision a life where you are in control.
- Therapy goals: By setting and achieving small goals, you begin to feel more hopeful about recovery.
- Successes: Celebrating each triumph, no matter how minor, reinforces your belief in the possibility of change.
Coping Skills: Strategies to handle emotional turmoil are essential. Your therapist can work with you to develop a toolkit of skills tailored to your needs.
- Mindfulness: Remaining present can reduce the intensity of negative emotions.
- Emotion regulation: Techniques like deep breathing can help manage sudden surges of emotion.
Takeaway: Combining optimism and practical coping strategies can significantly enhance recovery.
Support Systems and the Role of Loved Ones
When someone battles with self-destructive behavior linked to BPD, those closest to them play a crucial part. Family members, friends, and significant others offer a support network that promotes healing and contributes to a stable, nurturing environment.
Engaging Family and Friends
Family and friends carry great power in their ability to offer support. Here’s how they can engage effectively:
- Listen Actively: Show that you hear and understand by providing your full attention.
- Educate Themselves: Knowledge about BPD can help in responding to challenges compassionately.
- Set Boundaries: Support needs to be consistent but not at the cost of personal well-being.
By participating in treatment discussions and understanding triggers, loved ones can help navigate the journey to stability.
Key Takeaway: Actively involving family and friends in a supportive role can enhance the treatment process.
Creating a Safe and Stable Environment
A safe and stable environment is vital for someone with BPD to manage self-destructive tendencies. Here’s what can help:
- Consistency: Routine and predictability can reduce stress and confusion.
- Open Communication: Encourage honest and respectful dialogue to address concerns.
- Positive Reinforcement: Acknowledging progress, however small, reinforces self-worth.
Significant others and close family members who maintain a calm and secure space contribute significantly to the overall stability of someone with BPD.
Key Takeaway: Providing a consistent, safe environment helps individuals with BPD feel secure and supported.
Long-term Management and Future Outlook
Effective long-term management of self-destructive behaviors in Borderline Personality Disorder (BPD) is vital to ensure future stability and success. Let’s explore strategic approaches and how to maintain progress through life’s inevitable changes.
Developing Long-term Management Strategies
To chart a course for success, you need a solid plan. Here’s where to begin:
- Identify Triggers: Keep a journal to note what sparks your self-destructive behaviors. Awareness is the first step in long-term management.
- Seek Regular Therapy: Engage with therapies that benefit BPD, like Dialectical Behavior Therapy (DBT) or Cognitive Behavioral Therapy (CBT).
- Build Support Networks: Surround yourself with friends, family, or support groups who understand your journey and offer encouragement.
Key Takeaway: Your compass for navigating BPD is your detailed plan that includes self-awareness, professional guidance, and community support.
Adapting to Life Changes and Maintaining Progress
Life is full of twists and turns. Managing BPD is about adapting while keeping your eyes on the prize. Here’s how:
- Continual Learning: Embrace new coping strategies as you grow. What works now may need tweaking in the future.
- Celebrate Small Wins: Recognize and savor each step forward. Progress might be slow, but it’s still progress!
- Stay Proactive: Regular check-ins with mental health professionals can help you stay on track despite life’s changes.
Key Takeaway: Embracing adaptability and celebrating every victory, no matter how small, are essential in maintaining your progress with BPD.
Resources and Helpful Information
Navigating life with borderline personality disorder can be challenging, but you’re not alone. A wealth of resources and support systems are ready to aid in your journey toward wellness.
Educational Materials and Support Groups
Educational Materials:
- Books: I Hate You—Don’t Leave Me; The Borderline Personality Disorder Survival Guide
- Online Resources: National Education Alliance for Borderline Personality Disorder (NEABPD) Website
- Videos & Webinars: NEABPD’s free educational videos
Support Groups:
- In-person Meetings: Local mental health clinics and community centers often host BPD support groups.
- Online Forums: Forums such as BPDfamily.com, where you can share experiences and tips.
Key Takeaway: Knowledge is power; connecting with others can provide comfort and insight.
 Accessing Professional Help and Treatment Centers
Accessing Professional Help and Treatment Centers
- Therapists: Look for professionals specializing in dialectical behavior therapy (DBT).
- Psychiatrists: Can prescribe and manage medication that might help manage BPD symptoms.
Treatment Centers:
- Residential Programs: Facilities like Clearview Women’s Center offer specialized BPD treatment.
- Day Treatment: Intensive outpatient programs that offer structure and support without full hospitalization.
Key Takeaway: Professional support can be a lifeline, with treatment tailored to your unique needs.
Frequently Asked Questions
Navigating through borderline personality disorder (BPD) often means tackling self-destructive behaviors head-on. This section provides targeted insights that can support you or someone you know in understanding and managing these challenging actions.
How can someone with BPD recognize and address self-destructive behaviors?
You might notice patterns of behavior that cause personal harm or distress in various aspects of your life. Acknowledging these actions as part of BPD is a critical first step. After recognition, seeking professional guidance can pave the way forward.
Key takeaway: Early recognition followed by professional help is essential for addressing self-destructive behaviors.
What types of treatment are effective for managing self-destructive tendencies in BPD?
Evidence-based therapies like Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT) are effective. These treatments can guide you in understanding the root cause of your actions and develop healthier coping mechanisms.
Key takeaway: Therapies such as DBT and CBT are powerful tools for managing self-destructive behaviors in BPD.
Are there coping strategies that can help reduce self-harm in individuals with borderline personality disorder?
Yes, there are several strategies you can adopt:
- Mindfulness exercises to ground your emotions
- Establishing a support network of friends or support groups
- Engaging in physical activities to release built-up tension
Key takeaway: Adopting healthy coping strategies can significantly reduce instances of self-harm.
How do self-destructive actions in BPD affect relationships, and how can they be handled?
Self-destructive actions may lead to strained relationships and mistrust. Communication is key—expressing your struggles to loved ones can help them understand and support you. Setting boundaries and working on your behaviors with a therapist can improve relationships.
Key takeaway: Open communication and professional guidance are vital in mitigating the strain on relationships.
What is the role of therapy in helping someone with borderline personality disorder overcome self-destructiveness?
Therapy serves as a cornerstone in combating self-destructiveness. A therapist can guide you through understanding your triggers and developing coping mechanisms to resist harmful impulses.
Key takeaway: Therapeutic intervention is critical in overcoming self-destructive patterns in BPD.
Can lifestyle changes contribute to reducing self-destructive behaviors in people with BPD?
Absolutely, embracing lifestyle changes such as getting proper sleep, maintaining a balanced diet, and reducing substance use can have a substantial impact. These changes bolster your physical and mental health, making it easier to manage BPD symptoms.
Key takeaway: Lifestyle adjustments can play a supporting role in curbing self-destructive behaviors in BPD.
- Breaking the Silence: Why Men’s Mental Health Matters More Than Ever - April 15, 2025
- How to Transform a Home’s Patio Space into a Relaxing Space - March 23, 2025
- 5 Strategies to Use a Cell Phone to Help Manage Your Stress - March 23, 2025
This site contains affiliate links to products. We will receive a commission for purchases made through these links.


 Understanding Borderline Personality Disorder
Understanding Borderline Personality Disorder Causes and Contributing Factors
Causes and Contributing Factors Manifestations of Self-Destructive Behavior
Manifestations of Self-Destructive Behavior Emotional Dysregulation and Interpersonal Relationships
Emotional Dysregulation and Interpersonal Relationships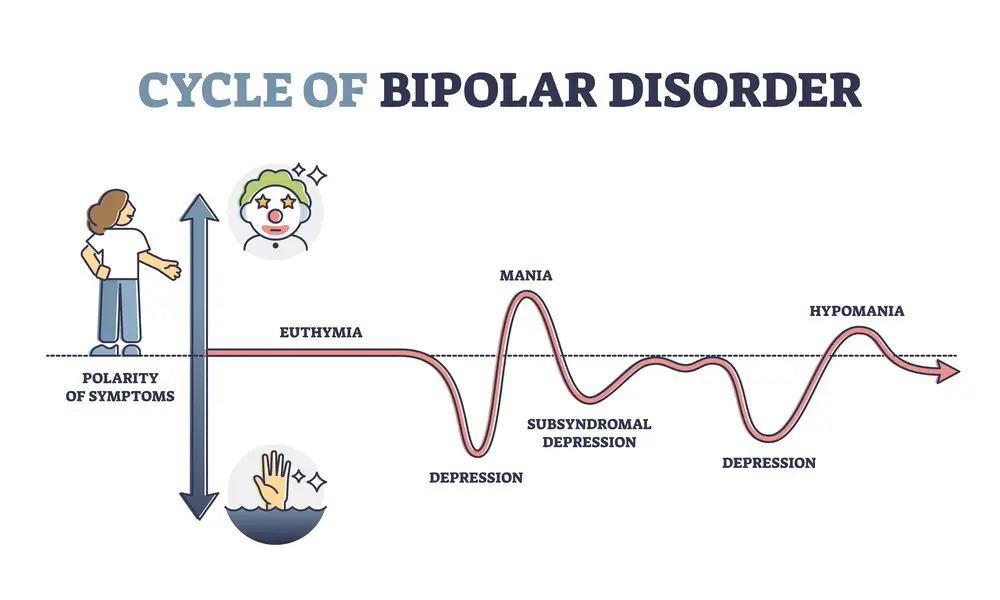 Distinguishing BPD from Similar Conditions
Distinguishing BPD from Similar Conditions Accessing Professional Help and Treatment Centers
Accessing Professional Help and Treatment Centers
