As a BetterHelp affiliate, we receive compensation from BetterHelp if you purchase products or services through the links provided
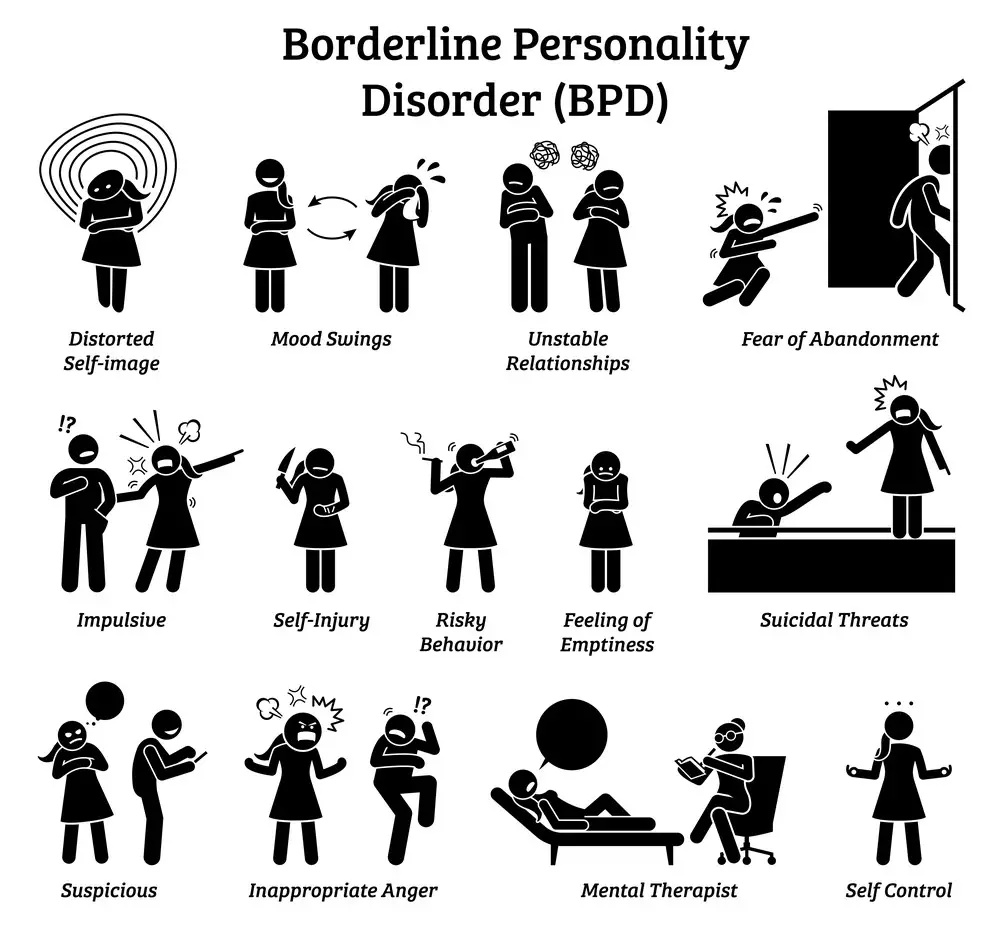
Borderline personality disorder (BPD) is a complex mental health condition characterized by intense emotions, difficulty in maintaining relationships, and a distorted self-image. It’s one of several personality disorders recognized by mental health professionals and can have a profound impact on your life. Understanding BPD is crucial as it affects how you think, feel, and interact with others, often leading to patterns of instability in behavior and relationships.
While the core features of BPD are similar, the disorder can manifest in different subtypes, each with its pattern of thoughts and behaviors. This variability presents a challenge in diagnosis and treatment, making it essential to recognize the nuances of the condition. Knowledge about the types of BPD aids in not only better diagnosis but also in developing tailored treatment plans that address your specific needs, helping you to manage symptoms more effectively.
Therapeutic approaches and coping strategies are key components when managing BPD. Treatment is primarily focused on psychotherapy but may also include medication. Through therapy, you can learn to manage emotions and reduce impulsive behaviors, improving relationships and providing greater control over your life. With education, support, and effective management strategies, many individuals with BPD experience significant improvements.
Key Takeaways
- BPD is a significant mental health condition with varying manifestations.
- Identifying the type of BPD is vital for creating an effective treatment plan.
- Therapeutic strategies are central to managing BPD symptoms and improving quality of life.
- These subtypes are not exclusive or exhaustive.
 Understanding BPD
Understanding BPD
Borderline Personality Disorder (BPD) is a complex mental health condition that significantly impacts a person’s life. Grasping its definition and the scope of its prevalence offers crucial insights.
Defining BPD
Borderline Personality Disorder is a type of personality disorder characterized by difficulties in regulating emotions. This results in severe, unstable mood swings, impulsivity, and a poor self-image. BPD often results in issues with maintaining relationships, and challenges in everyday activities may arise. A diagnosis is typically based on a pattern of interactions and behaviors inconsistent with the individual’s cultural expectations and pervasive, inflexible, and enduring.
- Symptoms usually appear in adolescence or early adulthood.
- Diagnosis involves a thorough clinical interview, psychological assessment, and consideration of the individual’s history.
Prevalence and Demographics
Statistics reveal that about 1.4% of the adult population is affected by BPD, with the condition being more common among women than men. The prevalence can vary, but it is crucial to recognize that BPD touches people across all demographics regardless of age, gender, race, or social status.
- Women are diagnosed with BPD more frequently, constituting about 75% of diagnosed cases.
- Symptoms can manifest from adolescence and are typically diagnosed in early adulthood.
| Demographics | Percent Affected |
|---|---|
| Adult Population | 1.4% |
| Gender (Women) | 75% |
Key Takeaway: Recognizing the prevalence of BPD in different demographics can enhance awareness and empathy, fostering a better understanding of the needs of those affected by this mental health condition.
 Causes of BPD
Causes of BPD
Borderline Personality Disorder (BPD) can stem from a complex interplay of factors. Understanding these can help you piece together the puzzle of what contributes to the development of this condition.
Genetics
Your genes may play a significant role in the likelihood of developing BPD. Studies point out that if a close family member has BPD, your chances of having the condition increase. This doesn’t mean it’s a certainty – instead, it’s a piece in the larger mosaic of causes:
- Heredity: The chance of having BPD is higher if there’s a family history of the disorder.
- Specific Genetic Factors: Research is ongoing to pinpoint which genes contribute and how they interact with other causes.
Environmental Factors
The environment in which you grow up can substantially influence your development of BPD. Stressful, unstable, or chaotic family environments can be particularly impactful:
- Stress and Trauma: Persistent exposure to stressful situations or significant trauma, especially during formative years, can heighten your risk.
- Abuse: Histories of physical, emotional, or sexual abuse are common among those with BPD.
Childhood and Development
Your experiences as a child can leave lasting impressions that affect the development of BPD. Instances of trauma or difficulty during childhood have been noted as potential triggers:
- Neglect: Emotional neglect can disrupt the development of secure attachments and self-image.
- Early Parental Loss: Loss or separation from caregivers could contribute to fears of abandonment, which feature in BPD.
Key Takeaway: Genetics, environmental factors, and childhood experiences each play a crucial part in the development of BPD. A better grasp of these can improve understanding and support for those affected.
Types of BPD
Borderline Personality Disorder (BPD) is a complex mental health condition marked by emotional instability, difficulties in maintaining relationships, and intense fear of abandonment. Theodore Millon identified various subtypes that help understand the different behavior patterns in individuals with BPD. Each subtype has unique characteristics that set it apart.
1. Impulsive BPD
You might recognize Impulsive BPD by the tendency for quick actions and rapid mood changes. If you have this subtype, you may:
- Act spontaneously, often without considering the consequences.
- Exhibit an energetic, charismatic demeanor.
Key Takeaway: Impulsive BPD involves high energy and unpredictable behavior.
2. Discouraged BPD
With Discouraged BPD, feelings of dependency and a deep fear of being alone can prevail. Your behaviors may include:
- Clinging to others and going to great lengths to avoid rejection.
- Displaying a submissive and self-deprecating attitude.
Key Takeaway: Those with Discouraged BPD often experience intense feelings of abandonment.
3. Petulant BPD
Petulant BPD can be paradoxical, where you struggle with feelings of unworthiness alongside a compulsion to assert control. Key signs are:
- Displaying passive-aggressive behaviors.
- Experiencing unpredictability in moods and actions.
Key Takeaway: If Petulant BPD resonates with you, you may vacillate between anger and guilt.
4. Self-Destructive BPD
In Self-Destructive BPD, self-harm and reckless behaviors might be a distressing reality. This can include:
- Engaging in self-sabotage when things seem to go well.
- Exhibiting a persistent disregard for your safety.
Key Takeaway: Self-Destructive BPD is characterized by a harmful pattern towards oneself.
5. Self-Deserting BPD
- Characteristics: Individuals with this subtype may dissociate or detach from their identities and experiences. They often feel numb or disconnected from their emotions.
- Behaviors: This can lead to zoning out, losing track of time, and an unstable self-image.
- Key Takeaway: Self-deserting BPD often involves a disconnect from one’s self, leading to a sense of emptiness or depersonalization.
6. Eccentric BPD
- Characteristics: This subtype is marked by odd, quirky behaviors or thinking. People might exhibit unusual beliefs or superstitions.
- Behaviors: They may also have unconventional ways of relating to others and seem distant or detached.
- Key Takeaway: Eccentric BPD involves unconventional thinking and behaviors, often leading to a sense of being different or misunderstood.
7. Anxious BPD
- Characteristics: Here, anxiety and nervousness are predominant. Individuals may be plagued by constant worries and fears, especially about relationships.
- Behaviors: They often seek reassurance and may be sensitive to perceived criticism or rejection.
- Key Takeaway: Anxious BPD is characterized by pervasive anxiety, especially concerning relationships and self-image.
8. Nonconforming BPD
- Characteristics: This subtype is characterized by a strong resistance to societal norms and expectations.
- Behaviors: Individuals may rebel against authority or convention, often expressing themselves in unique or unconventional ways.
- Key Takeaway: Nonconforming BPD involves a distinct resistance to conforming, with a preference for individuality and uniqueness.
9. Placating BPD
- Characteristics: Individuals with this subtype tend to be overly accommodating and yielding to others, often at the expense of their own needs.
- Behaviors: They may struggle to assert themselves and tend to prioritize others’ needs over their own.
- Key Takeaway: Placating BPD is marked by a constant effort to please others, often leading to self-neglect and a loss of personal identity.
 Signs and Symptoms
Signs and Symptoms
Borderline Personality Disorder (BPD) manifests through a range of signs and symptoms that can significantly impact your life. Here, you’ll learn about the crucial aspects: emotional instability, impulsive behaviors, challenges in interpersonal relationships, and erratic self-image and identity.
Emotional Instability
Mood Swings: You might experience intense and rapid mood shifts, often without a clear trigger. These can include:
- Feelings of intense happiness or euphoria
- Sudden anger or irritability
- Profound sadness or anxiety
Feelings of Emptiness: A chronic sense of emptiness often accompanies these mood variations, leaving you feeling hollow inside.
Key Takeaway: Your emotions can feel like an unpredictable roller-coaster, which is not only disorienting for you but may also affect those around you.
Impulsive Behaviors
Risky Activities: Impulsivity may manifest in potentially harmful behaviors, such as:
- Spending sprees
- Unsafe sexual encounters
- Substance abuse
Anger Issues: You might also display intense anger or have trouble controlling your temper, even over minor issues.
Key Takeaway: Impulsive actions can lead to consequences that affect many areas of your life, and recognizing these tendencies is a step toward managing them.
 Interpersonal Relationships
Interpersonal Relationships
Fear of Abandonment: Even a hint of separation or rejection can lead to drastic efforts to prevent this abandonment.
Unstable Relationships: Your relationships can swing between idealization and devaluation—someone may be the most significant person in your eyes one day and the worst the next.
Key Takeaway: Navigating relationships can feel like navigating a minefield, where you’re constantly looking for potential threats.
Self-Image and Identity
Shifting Sense of Self: You might find your sense of self is unstable; for example:
- Changing goals, values, and aspirations frequently without a clear direction
- Shifting opinions and views about yourself and your role in the world
Chronic Insecurity: Feelings of uncertainty and self-doubt can make it difficult for you to maintain a consistent image of who you are.
Key Takeaway: Building a stable self-image is a complex journey central to managing BPD.
 Associated Conditions
Associated Conditions
Borderline personality disorder (BPD) often coexists with other mental health conditions, which can complicate the diagnosis and treatment. Understanding these associated conditions is crucial for comprehensive care.
Mood and Anxiety Disorders
Individuals with BPD may also struggle with mood disorders, such as bipolar disorder, which can cause dramatic mood swings ranging from depressive lows to manic highs. Additionally, various anxiety disorders are common, including generalized anxiety disorder, panic disorder, and social anxiety disorder.
Key Takeaway: Mood and anxiety disorders can exacerbate BPD symptoms, requiring integrated treatment approaches.
Eating Disorders
Eating disorders, like bulimia and anorexia, are more prevalent among those with BPD. These conditions involve a chronic disruption of eating behaviors and are linked to an intense concern with body image and weight.
Key Takeaway: Recognizing and treating eating disorders alongside BPD is vital, as they can have severe emotional and physical health consequences.
Substance Use Disorders
Substance use disorders (SUD) often occur with BPD. Patterns of substance abuse appear as coping mechanisms for emotional pain but, unfortunately, lead to additional health and psychosocial issues.
Key Takeaway: Addressing SUD in the context of BPD is crucial because it impacts recovery and quality of life.
Post-Traumatic Stress Disorder (PTSD)
Many individuals with BPD have experienced trauma, leading to PTSD. Symptoms of PTSD, such as flashbacks, avoidance, and hyperarousal, can overlap and intensify the symptoms of BPD.
Key Takeaway: Treatment for BPD should include interventions for PTSD when present to aid in the healing process.
Diagnosis of BPD
Borderline Personality Disorder (BPD) diagnosis relies on a careful psychological assessment and a detailed evaluation of symptoms. It’s a nuanced process that distinguishes BPD from other personality disorders.
Criteria and Evaluation
The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) provides the diagnostic criteria for BPD. Your mental health professional will evaluate your symptoms against these standards:
- Persistent emotional instability: You might experience intense mood swings.
- Impaired interpersonal relationships: Relationships often appear tumultuous.
- Identity disturbance: A markedly and persistently unstable self-image or sense of self.
- Impulsivity: This is often in areas that are potentially self-damaging.
- Recurrent suicidal behavior, gestures, or threats: Any self-harming behavior fits into this category.
- Chronic feelings of emptiness: A pervasive sense of nothingness or boredom.
- Inappropriate, intense anger: Difficulties controlling anger are common.
- Transitory, stress-related paranoia or severe dissociative symptoms: Periods of paranoia or dissociation may occur.
Key takeaway: Accurate diagnosis involves a thorough evaluation using the DSM-5 criteria to identify hallmark symptoms of BPD, often through discussions about your emotional experiences, thoughts, and behaviors.
Differential Diagnosis
Distinguishing BPD from other personality disorders is imperative for proper treatment. Your mental health provider may explore other conditions to rule out or identify co-occurring disorders:
- Narcissistic Personality Disorder: Unlike BPD, it’s characterized by enduring patterns of grandiosity and a lack of empathy.
- Antisocial Personality Disorder: This involves a disregard for social norms and the rights of others, which is not a focus in BPD diagnosis.
- Histrionic Personality Disorder: While it shares emotional instability with BPD, it’s distinct in its pattern of excessive attention-seeking behaviors.
Bipolar Disorder Differentiation: Sometimes, bipolar disorder can be confused with BPD due to mood instability, but they differ in the duration and origin of mood episodes.
Anxiety and Mood Disorders: These may coexist with BPD but are differentiated by the nature and duration of symptoms.
Key takeaway: A differential diagnosis ensures that your symptoms are not better explained by another condition, confirming a BPD diagnosis and guiding the course of your treatment.
 Treatment Approaches
Treatment Approaches
When tackling Borderline Personality Disorder (BPD), it’s essential to understand the variety of treatment options available to you. These approaches are tailored to manage symptoms and improve quality of life, emphasizing mental wellness and emotional resilience.
Psychotherapy
Psychotherapy, often the cornerstone of treatment for BPD, revolves around counseling sessions with trained therapists. Here’s a breakdown of what this involves:
- Individual Therapy: One-on-one sessions focus on understanding your emotions and behaviors while building new coping mechanisms.
- Group Therapy: Provides a supportive environment where you can share experiences and learn from others with BPD.
Key Takeaway: Psychotherapy aims to delve into emotional patterns, offering strategies to handle and modify them.
Medications
Although no medication specifically treats BPD, certain drugs can help manage co-occurring symptoms or conditions, such as:
- Mood Stabilizers: To reduce mood swings and emotional instability.
- Antidepressants: May alleviate feelings of depression or anger.
- Antipsychotics: Sometimes used if symptoms include distorted thinking or perception.
Key Takeaway: Medications can be prescribed to address specific symptoms, but they’re most effective when combined with therapy.
 Dialectical Behavior Therapy (DBT)
Dialectical Behavior Therapy (DBT)
DBT is a form of psychotherapy uniquely suited for BPD and includes:
- Mindfulness: Learning to be present in the moment.
- Distress Tolerance: Coping with stress without resorting to self-destructive behaviors.
- Emotional Regulation: Understanding and managing intense emotions.
- Interpersonal Effectiveness: Navigating relationships more healthfully.
Key Takeaway: DBT equips you with practical skills to manage emotions and improve relationships.
Managing Relationships
In navigating borderline personality disorder (BPD), managing your relationships is a crucial step toward creating a healthier, more stable environment for yourself and your loved ones.
Personal Relationships
Your relationships can be vibrant and intense, often reflecting your deep capacity for connection. To maintain the health of these relationships, it’s essential to:
- Communicate Openly: Keep an open line of communication with friends and family. Express your feelings and needs clearly and listen to theirs as well.
- Seek Understanding: Try to understand the perspective of others. Remember, it’s not just about how you feel but also about mutual respect and appreciation.
Key Takeaway: Open communication and seeking understanding are vital in nurturing personal relationships.
 Setting Boundaries
Setting Boundaries
Establishing boundaries is essential to any healthy relationship, particularly when you’re prone to experiencing intense emotions.
- Identify Your Limits: Reflect on what you can tolerate and accept—and what makes you uncomfortable or stressed.
- Be Assertive: Convey your boundaries to others. It is okay to say ‘no’ or ‘stop’ when something crosses your line.
- Expect Respect: Those who care for you should honor your boundaries. Understanding and respect go both ways.
Key Takeaway: Identifying and asserting your boundaries is fundamental to any healthy relationship.
Building Stability
A sense of stability in your relationships can help counteract the fear of abandonment that is often experienced with BPD.
- Routines and Commitments: Establish routines or regular commitments with loved ones to deepen trust and predictability in your relationships.
- Support Networks: Cultivate a diverse range of supportive connections. This could include family, friends, therapists, or support groups.
Key Takeaway: Building stability through routines and a diverse support network can create a more secure environment, reducing the fear of abandonment.
Coping Strategies
Coping strategies are essential tools for managing the symptoms of BPD. They can help you stabilize your emotions and respond to stress more effectively.
Emotion Regulation
You can think of emotion regulation as the process of managing and responding to intense emotions without getting overwhelmed. It’s crucial to have a strategy that works for you. Here are some practical steps:
- Identify and label your emotions: Recognize and acknowledge what you’re feeling.
- Practice opposite actions: If you feel like lashing out, try to do something calming instead.
Key Takeaway: Learning to regulate your emotions helps prevent impulsive actions.
Distress Tolerance
When stress hits, it’s typical to want to escape it, but that’s not always possible or healthy. Distress tolerance is about surviving those tough moments without making them worse.
- Distract yourself with positive activities: Engage in hobbies or exercises you enjoy.
- Use self-soothing techniques: This could be deep breathing, taking a bath, or listening to calming music.
Key Takeaway: Building tolerance to distress allows you to move through challenging times without adding to your stress.
 Mindfulness
Mindfulness
Mindfulness is the practice of being fully present in the moment. It is a powerful tool that can help reduce impulsivity.
- Focus on your breath: This simple act can ground you and bring you back to the present moment.
- Observe without judgment: Pay attention to your thoughts and feelings without labeling them as good or bad.
Key Takeaway: Mindfulness can improve your mental health by helping you focus on the present rather than being caught up in past or future worries.
Incorporating these strategies into your life may take time and effort. Remember to reach out to a mental health professional to guide you through the process and develop a treatment plan that’s tailored to your needs.
Living with BPD
Living with Borderline Personality Disorder (BPD) means navigating daily life with a mental health condition that influences your feelings, behavior, and relationships. Consistent, long-term management is crucial to maintaining stability and enhancing quality of life.
Quality of Life
- Stability: Your emotional and behavioral stability is key. Strategies like mindfulness and therapy can create a more predictable life experience.
- Functioning: Day-to-day functioning can be hard with BPD. Treatment often focuses on skills training to improve emotional regulation and interpersonal effectiveness.
Key Takeaway: A structured routine and coping strategies can significantly improve stability and functioning.
Long-Term Management
- Treatment Plan: Stick with a comprehensive treatment plan, including therapy and medication, to maintain progress and manage symptoms.
- Health: Prioritize your overall health. Regular exercise, sufficient sleep, and a balanced diet contribute to both physical and mental wellness.
Key Takeaway: Consistency in following your treatment plan is vital for long-term management.
Support Networks
- Support: Cultivate a strong network. Family, friends, and support groups can provide invaluable support and understanding.
- Professional Help: Maintain regular contact with healthcare professionals. They can offer guidance and adapt your treatment as needed.
Key Takeaway: Remember, you’re not alone. Leverage your support networks to stay grounded and receive the help you need.
Frequently Asked Questions
Borderline Personality Disorder (BPD) is a complex mental health condition with various subtypes, each presenting unique challenges and symptoms. Understanding these subtypes can be instrumental in seeking effective treatment and management strategies.
What are the recognized subtypes of Borderline Personality Disorder?
There are four commonly recognized subtypes of BPD: Impulsive, Petulant, Discouraged, and Quiet. Each subtype has distinctive traits and behaviors that affect how individuals experience and interact with the world around them.
Key takeaway: Knowing the specific BPD subtype can guide more personalized treatment approaches.
How does Quiet BPD differ from other forms of BPD?
Quiet BPD is characterized by internalizing struggles rather than externalizing them. You may direct the anger and impulsivity inward, which makes it less noticeable to others but equally painful for you. This can lead to isolation and loneliness, as the internal turmoil is less visible to the outside world than other subtypes.
Key takeaway: Quiet BPD may require careful observation and understanding as its symptoms are often concealed.
What characteristics are associated with the Impulsive subtype of BPD?
If you have the Impulsive subtype of BPD, you may exhibit highly spontaneous behaviors and tend to immediate gratification. Some of the hallmark characteristics include:
- Engaging in risky behaviors without considering the consequences.
- Sudden shifts in interests and friendships.
Key takeaway: Impulsivity can be thrilling but also comes with significant risks.
How can someone identify if they have the Discouraged variant of BPD?
The Discouraged variant of BPD often entails a pervasive sense of despondency. Individuals with this subtype:
- Might be prone to feelings of hopelessness and are heavily reliant on others for validation.
- Typically exhibit clingy and submissive behavior.
Key takeaway: Recognizing these signs can prompt you to seek support and avoid becoming excessively dependent on others.
What are common symptoms of Petulant BPD?
Petulant BPD can be particularly challenging due to a mix of anger, impatience, and unpredictability. Common symptoms include:
- Passive-aggressive behaviors.
- Difficulty with maintaining stable relationships due to unpredictable moods.
Key takeaway: Awareness of these symptoms is vital in managing interpersonal difficulties.
What are the potential risks and outcomes of untreated Borderline Personality Disorder?
Leaving BPD untreated can lead to a variety of negative outcomes, including:
- Increased risk of substance abuse and self-harm.
- Strain on personal and professional relationships.
Key takeaway: Timely intervention can significantly improve quality of life and prevent these risks.
- 3 Ways Wearing a Hat Can Help Lower Your Stress Levels - April 19, 2025
- Breaking the Silence: Why Men’s Mental Health Matters More Than Ever - April 15, 2025
- How to Transform a Home’s Patio Space into a Relaxing Space - March 23, 2025
This site contains affiliate links to products. We will receive a commission for purchases made through these links.


 Understanding BPD
Understanding BPD Causes of BPD
Causes of BPD Signs and Symptoms
Signs and Symptoms Interpersonal Relationships
Interpersonal Relationships Associated Conditions
Associated Conditions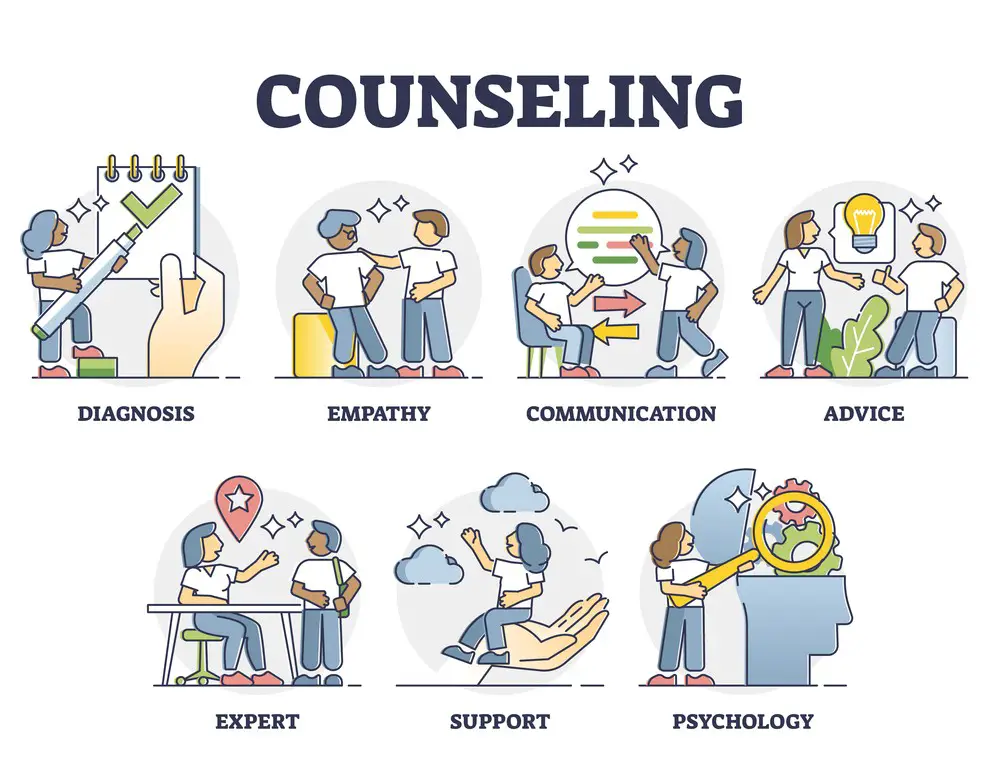 Treatment Approaches
Treatment Approaches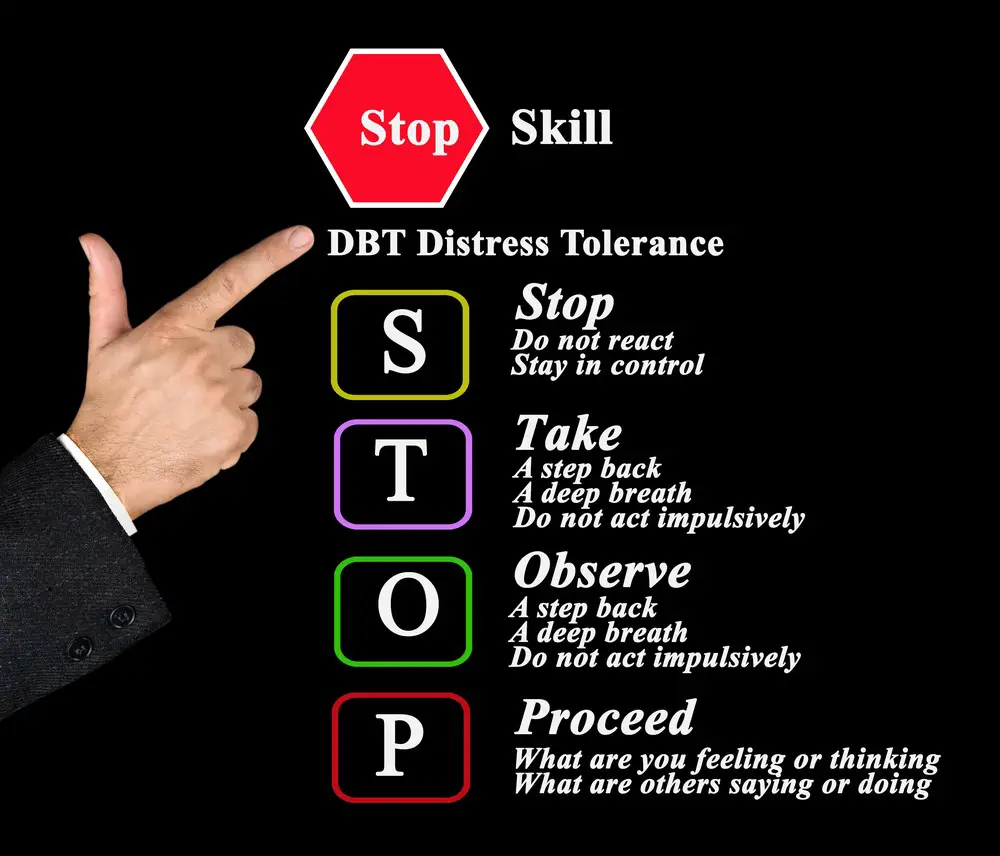 Dialectical Behavior Therapy (DBT)
Dialectical Behavior Therapy (DBT) Setting Boundaries
Setting Boundaries Mindfulness
Mindfulness
