As a BetterHelp affiliate, we receive compensation from BetterHelp if you purchase products or services through the links provided
In the ever-evolving field of mental health, three therapies have gained significant recognition—Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Acceptance and Commitment Therapy (ACT). Each approach offers unique methods to help individuals cope with various mental health issues, such as anxiety, depression, and borderline personality disorder. By exploring these mainstays of modern therapy, mental health professionals continue to refine and expand their understanding of human behavior and emotions.
CBT, the most well-known of these approaches, emphasizes identifying and challenging cognitive distortions to alter emotional responses and behaviors. DBT, a modification of CBT, focuses specifically on emotional regulation and interpersonal effectiveness, often utilized in treating borderline personality disorder. ACT, a newer, mindfulness-based therapy, helps individuals accept their thoughts and feelings instead of trying to change them and encourages commitment to personal values and goals. Through each therapeutic approach, mental health practitioners tailor their support to best address and treat their clients’ needs.
Key Takeaways
- The article discusses CBT, DBT, and ACT as prominent therapeutic approaches in mental health care.
- Each therapy is tailored to address different mental health issues with unique methods and tools.
- Understanding the effectiveness of these therapies enables mental health professionals to treat specific conditions better.
 Exploring Different Therapies
Exploring Different Therapies
Several types of evidence-based psychotherapies are available for individuals seeking mental health support. Three such therapies, which have gained popularity over the years, include Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Acceptance and Commitment Therapy (ACT). These talk therapies share some similarities but differ in their approach, techniques, and objectives.
Cognitive Behavioral Therapy (CBT) is a widely utilized therapy that focuses on identifying and changing dysfunctional thoughts, emotions, and behaviors. It emphasizes the connection between thoughts, feelings, and actions and assists individuals in developing practical skills to challenge negative thought patterns and replace them with healthier alternatives. CBT has been proven effective in treating various mental health conditions, such as anxiety, depression, and obsessive-compulsive disorder.
Dialectical Behavior Therapy (DBT) was originally developed as a specific treatment for individuals with borderline personality disorder but has since been adapted to address various psychological issues. DBT incorporates CBT elements and emphasizes accepting uncomfortable thoughts and feelings. It incorporates mindfulness, emotional regulation, and interpersonal effectiveness and is particularly effective in helping individuals manage intense emotions and impulsive behaviors and fostering healthier relationships.
Acceptance and Commitment Therapy (ACT) is a relatively newer form of therapy that, like DBT, incorporates mindfulness techniques. ACT encourages individuals to accept, rather than avoid, unwanted thoughts and emotions. It emphasizes developing psychological flexibility through recognizing and embracing one’s emotions and experiences and committing to actions that align with personal values and goals. This approach has effectively treated various conditions, such as depression, anxiety, and chronic pain.
In summary, CBT, DBT, and ACT are three evidence-based talk therapy options that successfully treat various mental health issues. Each therapy has distinct approaches and techniques, offering different pathways for individuals to achieve mental well-being and personal growth. Individuals must discuss their needs and preferences with a mental health professional to determine the most effective therapy for their unique circumstances.
Cognitive Behavioral Therapy (CBT)
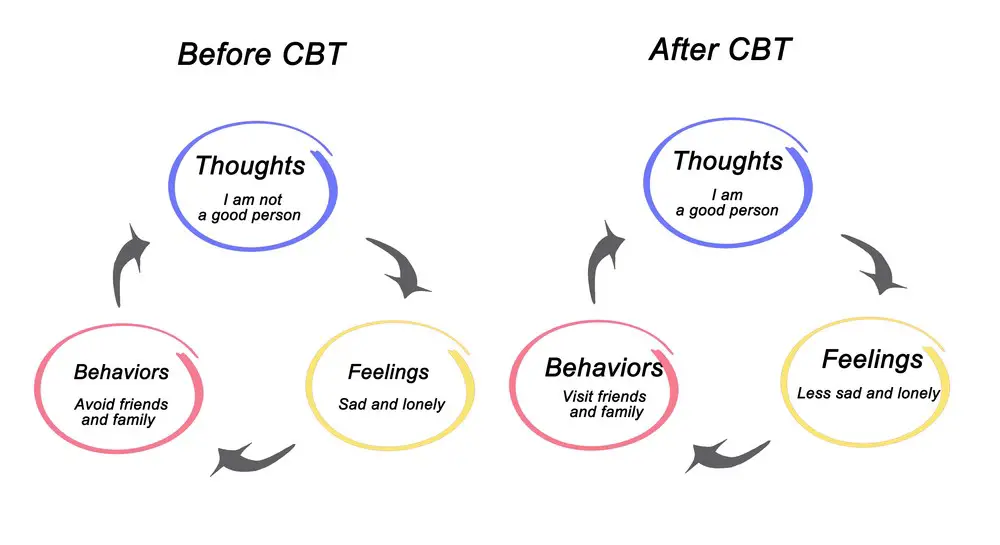 Cognitive Behavioral Therapy (CBT) is a widely recognized and effective form of psychotherapy. It focuses on identifying and changing negative thought patterns and behaviors individuals experience daily. By doing so, CBT aims to improve emotional regulation and promote healthy coping strategies in various situations.
Cognitive Behavioral Therapy (CBT) is a widely recognized and effective form of psychotherapy. It focuses on identifying and changing negative thought patterns and behaviors individuals experience daily. By doing so, CBT aims to improve emotional regulation and promote healthy coping strategies in various situations.
CBT primarily addresses clients’ automatic thoughts, which are the spontaneous and often negative thoughts that individuals experience in reaction to certain events, situations, or feelings. These thoughts can harm mental health, leading to anxiety, depression, and other psychological issues. CBT practitioners utilize cognitive therapy and behavior change strategies to help clients reframe these negative thoughts and develop healthier thinking patterns.
Cognitive therapy techniques used in CBT include:
- Thought recording: Clients are taught to identify and record automatic thoughts, allowing them to become more aware of negative thinking patterns and challenge them effectively.
- Cognitive restructuring: Clients learn to replace maladaptive thoughts with healthier, more balanced alternatives, improving emotional well-being.
Behavior change strategies employed in CBT involve:
- Behavioral activation: Clients are encouraged to engage in activities and hobbies that bring them pleasure or a sense of accomplishment to counteract feelings of depression or anxiety.
- Exposure therapy: Clients confront and gradually face their fears and anxiety-provoking situations, reducing the intensity of their reactions over time.
It is important to note that CBT is a flexible approach, with therapists often tailoring the techniques used based on the individual’s specific needs and goals. Furthermore, CBT has been proven effective in treating various mental health disorders such as anxiety, depression, post-traumatic stress disorder (PTSD), and obsessive-compulsive disorder (OCD).
In conclusion, Cognitive Behavioral Therapy is a well-established, evidence-based treatment that focuses on changing unhelpful thoughts and behaviors to improve mental health and overall well-being. Its techniques are adaptable to individual needs, and it has been proven effective in treating various psychological issues.
Dialectical Behavior Therapy (DBT)
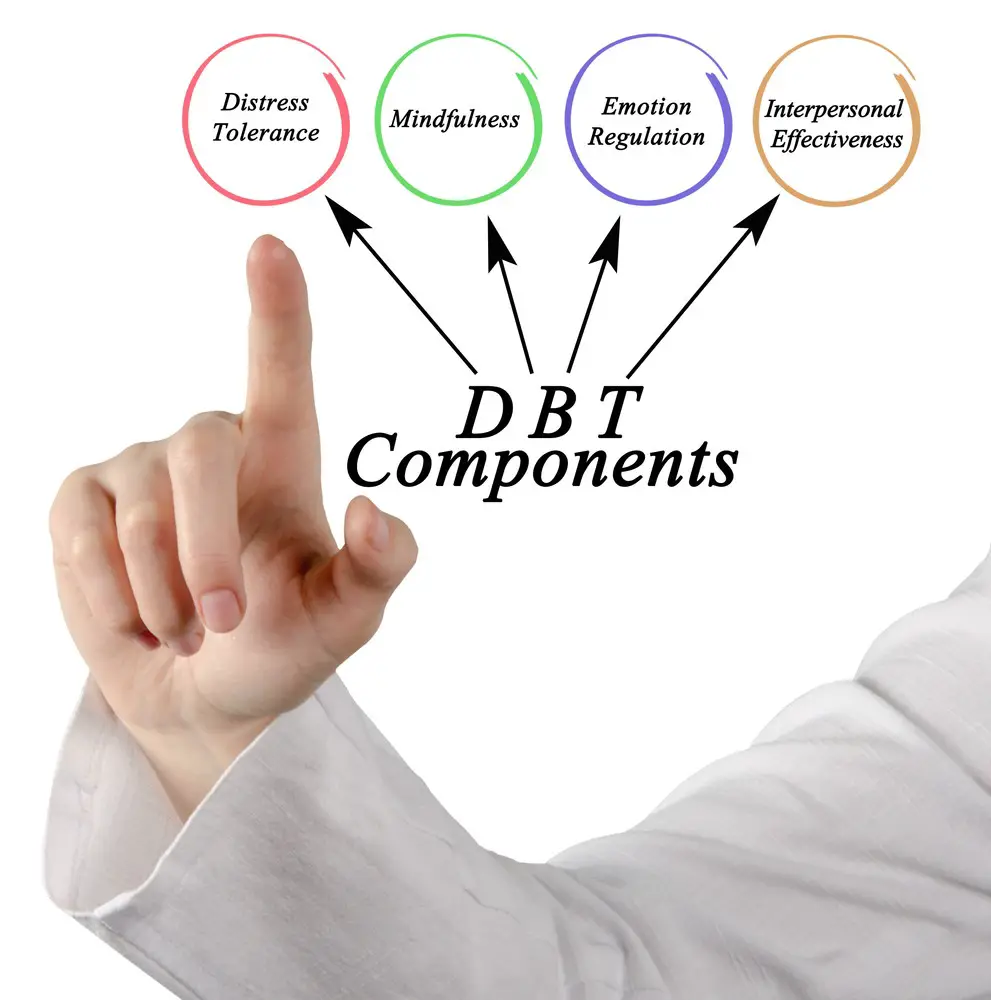
Dialectical Behavior Therapy (DBT) is a cognitive-behavioral therapy developed by psychologist Marsha Linehan in the late 1980s. It was originally designed to treat individuals with borderline personality disorder but has since been adapted and used for various mental health disorders and emotional challenges. DBT combines standard cognitive-behavioral techniques with mindfulness, acceptance, and dialectical strategies that harmonize change and acceptance.
DBT has four main components: interpersonal effectiveness, emotional regulation, distress tolerance, and mindfulness. These components help individuals learn more effective ways to manage relationships, control emotions, cope with difficult situations, and develop greater self-awareness.
Interpersonal Effectiveness teaches individuals how to communicate assertively, maintain self-respect, and navigate relationships effectively. Skills learned include setting boundaries, making requests, and dealing with interpersonal conflicts.
Emotional Regulation aims to help individuals recognize and manage their emotions. Techniques include identifying emotions, challenging negative beliefs, and learning coping strategies for handling emotional situations healthily.
Distress Tolerance teaches strategies for coping with difficult emotions and situations without resorting to destructive behaviors. This component includes crisis survival skills, such as self-soothing, distraction, and acceptance.
Mindfulness encourages awareness and acceptance of thoughts, emotions, and bodily sensations without judgment. Mindfulness practices like meditation and mindfulness exercises are integrated into DBT treatment to help individuals develop non-judgmental self-awareness.
In DBT, individuals typically participate in individual and group therapy sessions, which focus on building these skills. The goal is to help individuals develop more effective strategies for managing their emotions and behaviors, leading to improved mental health and overall well-being. While DBT is not a cure-all, it has shown effectiveness in treating various disorders and is an important tool in psychotherapy.
Acceptance and Commitment Therapy (ACT)
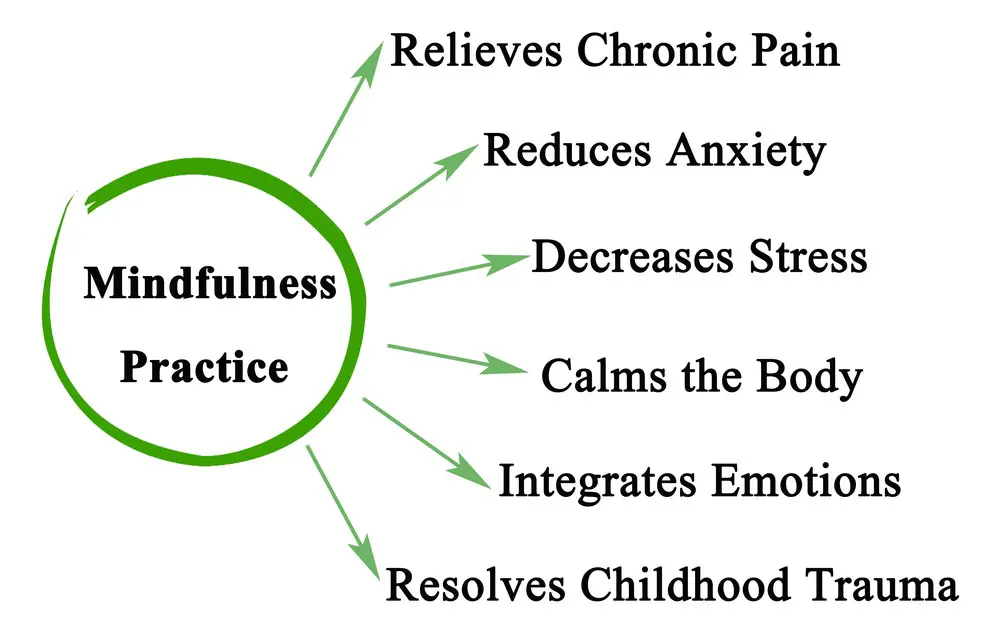 Acceptance and Commitment Therapy (ACT) is a form of psychotherapy that emphasizes psychological flexibility and helps individuals align their behavior with their core values. It combines acceptance and mindfulness strategies alongside commitment and behavior change techniques.
Acceptance and Commitment Therapy (ACT) is a form of psychotherapy that emphasizes psychological flexibility and helps individuals align their behavior with their core values. It combines acceptance and mindfulness strategies alongside commitment and behavior change techniques.
In ACT, acceptance involves embracing thoughts and feelings without trying to alter or eliminate them. This approach helps individuals to face uncomfortable situations rather than avoiding them. Being present and nonjudgmental allows individuals to adapt to their emotions without becoming overwhelmed.
Commitment is another essential aspect of ACT. This component encourages individuals to identify their core values and commit to actions aligning with them. By doing so, individuals can find meaning in their lives and reduce the impact of negative thoughts and emotions.
Cognitive defusion is a key technique used in ACT. It involves separating oneself from one’s thoughts and learning to see them as transient events that arise and disappear over time rather than as absolute truths. This aids in reducing the negative impact of harmful thoughts and beliefs.
Psychological flexibility is the ultimate goal of ACT. It is the ability to adapt to changing circumstances, remain present, and be open to various experiences while pursuing one’s values. This flexibility allows individuals to cope effectively with life’s challenges and cultivate greater resilience.
Mindfulness techniques play a vital role in ACT as they help individuals to be more aware of their thoughts, feelings, and bodily sensations. This heightened awareness enables individuals to embrace change, detach from negative thought patterns, and engage in meaningful actions that align with their values.
In conclusion, Acceptance and Commitment Therapy encourages individuals to embrace their thoughts, emotions, and experiences while focusing on behavioral change and pursuing core values to enhance psychological flexibility and overall well-being.
Treating Specific Mental Conditions
 Mental health conditions encompass a wide range of disorders, including anxiety disorders, depression, borderline personality disorder, obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), addiction, relationship issues, substance use disorder, bipolar disorder, schizophrenia, personality disorders, psychosis, suicidal ideation, attention deficit hyperactivity disorder (ADHD), and fibromyalgia. Each of these conditions may require different treatment approaches, and three commonly used therapies are dialectical behavior therapy (DBT), cognitive-behavioral therapy (CBT), and acceptance and commitment therapy (ACT).
Mental health conditions encompass a wide range of disorders, including anxiety disorders, depression, borderline personality disorder, obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), addiction, relationship issues, substance use disorder, bipolar disorder, schizophrenia, personality disorders, psychosis, suicidal ideation, attention deficit hyperactivity disorder (ADHD), and fibromyalgia. Each of these conditions may require different treatment approaches, and three commonly used therapies are dialectical behavior therapy (DBT), cognitive-behavioral therapy (CBT), and acceptance and commitment therapy (ACT).
Anxiety and Depression: CBT is frequently employed to treat anxiety disorders and depression because it focuses on changing negative thought patterns and beliefs. This treatment approach has been found particularly effective for specific anxiety disorders such as generalized anxiety disorder, panic disorder, and social anxiety disorder. ACT can also help manage anxiety and depression by teaching individuals to accept negative thoughts without judgment and focus on their values and goals.
Borderline Personality Disorder: DBT was originally developed for treating borderline personality disorder. It combines CBT and mindfulness practices to target emotional dysregulation, self-destructive behaviors, and troubled interpersonal relationships. DBT emphasizes skill-building in mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness.
OCD, PTSD, and ADHD: CBT is widely used in treating OCD and PTSD, as it addresses maladaptive thought patterns and behaviors that contribute to these disorders. On the other hand, ADHD is mostly managed through medication and, if necessary, complemented by behavioral interventions or the organization and time management strategies found in CBT.
Addiction and Substance Use Disorders: CBT and ACT address addiction and substance use disorders. CBT identifies triggers, develops coping strategies, and fosters problem-solving skills. ACT, in contrast, targets psychological flexibility and supports individuals in making behavior changes that align with their values, which can aid in the recovery process.
Bipolar Disorder, Schizophrenia, and Psychosis: Medication management is typically the cornerstone of treatment for bipolar disorder, schizophrenia, and psychosis. However, CBT can be an adjunct treatment to help manage symptoms, improve functioning, and promote recovery. ACT can also be beneficial in teaching acceptance strategies and fostering a sense of purpose for individuals affected by these conditions.
Fibromyalgia and Suicidal Thoughts: ACT is gaining recognition as a treatment option for fibromyalgia and chronic pain by emphasizing the development of acceptance and mindfulness skills while encouraging value-driven actions. In cases where suicidal ideation is present, DBT provides therapeutic support to build skills in coping with emotional distress and reducing self-destructive behaviors.
 Methods and Tools in Therapy
Methods and Tools in Therapy
When comparing DBT, CBT, and ACT therapies, it’s important to examine the methods and tools each approach employs. All three techniques share certain aspects, such as helping the clients develop better-coping strategies and having unique individual approaches.
In DBT (Dialectical Behavior Therapy), the primary focus is on emotion regulation and behavior change. Clients are taught skills to enhance their emotional regulation, such as mindfulness practices, and are provided validation during the process. Group therapy sessions are often significant in DBT, focusing on improving skills like interpersonal relationships and adaptive techniques. This therapy is particularly effective for individuals dealing with substance abuse and self-harm.
On the other hand, CBT (Cognitive Behavioral Therapy) focuses primarily on changing thoughts and beliefs to facilitate a shift in behavior and emotional experiences. In CBT, the clients are guided to recognize thought patterns contributing to their distress and reassess those beliefs to increase their sense of control and well-being. Some techniques used in CBT include behavioral experiments, identification and reevaluation of maladaptive thoughts, and problem-solving strategies. CBT has been widely used for varying mental health conditions like anxiety, depression, and stress management.
ACT (Acceptance and Commitment Therapy) employs mindfulness and awareness techniques to help clients work on self-acceptance and behavior change. The main goal is to increase psychological flexibility – recognizing and accepting one’s thoughts, emotions, and sensations non-judgmentally. This therapy focuses on six core processes: defusion, acceptance, being present, values, committed action, and self-as-context. With the implementation of these processes, ACT aims to assist clients in developing a greater understanding of their internal experiences, enabling them to respond more effectively to life’s challenges.
Overall, all three therapies, DBT, CBT, and ACT, emphasize building resilience and skills to cope with various life issues effectively. While each employs distinct methods and tools, clients ultimately benefit from the practical approaches promoting improved mental and emotional health.
Famous Figures in Therapy
Marsha Linehan is a prominent figure in therapy, specifically for her development of Dialectical Behavior Therapy (DBT). Linehan, a psychologist and researcher, created DBT to treat individuals with Borderline Personality Disorder, who often struggle with intense emotions and self-destructive behaviors.
Another key figure in therapy is Aaron T. Beck, often considered the father of Cognitive Behavioral Therapy (CBT). Beck developed CBT in the 1960s as a more structured, short-term approach to therapy aimed at helping clients identify and change negative thought patterns. CBT is widely used globally to treat various mental health disorders, including depression, anxiety, and eating disorders.
In addition to Beck and Linehan, Steven C. Hayes played a significant role in developing Acceptance and Commitment Therapy (ACT). Hayes, a clinical psychologist, and professor, took a different approach to traditional CBT by emphasizing mindfulness, acceptance, and value-driven actions. ACT has proven effective in treating various mental health issues like anxiety, depression, and trauma.
Each of these therapists has significantly contributed to the evolving landscape of therapeutic approaches, providing diverse treatment options for those in need. Their DBT, CBT, and ACT work has helped countless people work toward mental health and emotional well-being.
 Understanding Therapy Effectiveness
Understanding Therapy Effectiveness
In psychotherapy, understanding the effectiveness of different therapeutic approaches is crucial to provide the best care for clients. Three common approaches – Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Acceptance and Commitment Therapy (ACT) – each have their evidence base and address a variety of issues.
When considering the evidence base, it is important to examine which types of issues each therapy treats most effectively. Research has indicated that CBT effectively addresses anxiety, depression, and relationship problems. DBT, originally developed for treating Borderline Personality Disorder, has expanded its focus to address a range of emotional regulation difficulties, including eating disorders and self-harm. ACT, a mindfulness-based therapy, has gained empirical support for its effectiveness in treating chronic pain, trauma, and substance use.
A key difference among these therapies lies in their strategies to address emotions. CBT focuses on identifying and challenging distorted thought patterns, thus, altering emotions, while DBT emphasizes developing skills to regulate emotions effectively. On the other hand, ACT promotes psychological flexibility by encouraging clients to accept and make room for uncomfortable emotions without needing to change or control them.
In addressing relationship issues, CBT examines unhealthy patterns of communication and problem-solving skills. DBT integrates interpersonal effectiveness training, which teaches skills to manage conflict, express needs assertively, and maintain healthy relationships. ACT fosters value-based living, emphasizing the importance of committing to actions aligned with one’s values, positively impacting relationships.
Dealing with avoidance is another important aspect of therapy. CBT tackles avoidance by exposing clients to feared situations while modifying maladaptive thoughts and behaviors. DBT addresses avoidance through skills training, mindfulness, and acceptance of painful emotions. ACT specifically targets experiential avoidance by developing mindfulness and acceptance skills, enabling clients to engage fully in the present despite discomfort.
Lastly, anger management is an essential component in many therapeutic interventions. In this context, CBT delved into understanding the triggers and thought patterns leading to anger and implementing cognitive restructuring and behavioral techniques to manage it. DBT incorporates emotion regulation skills to manage anger and reduce impulsive reactions. ACT seeks to promote psychological flexibility by allowing clients to understand the context and function of their anger without attempting to control or suppress it.
The effectiveness of CBT, DBT, and ACT varies depending on the specific issue being addressed and the individual client’s needs and preferences. Each of these approaches has strengths and an evidence base, making them valuable tools in psychotherapy.
Final Thoughts
DBT, CBT, and ACT are all evidence-based psychotherapy modalities that have demonstrated positive outcomes in treating various mental health issues. Each approach focuses on specific techniques and goals, allowing for the possibility of tailoring interventions to individual needs.
DBT (Dialectical Behavior Therapy) emphasizes the balance between acceptance and change, focusing on emotion regulation and interpersonal effectiveness. It is particularly useful for individuals with borderline personality disorder and other emotionally dysregulated clients.
CBT (Cognitive Behavioral Therapy) targets maladaptive thinking patterns and behaviors to change cognitive processes and behavioral responses. This approach has shown effectiveness in treating various mental health disorders, such as depression, anxiety, and obsessive-compulsive disorder.
ACT (Acceptance and Commitment Therapy) encourages clients to accept their thoughts and emotions without judgment while focusing on values-based action to improve their overall quality of life. ACT is helpful for individuals experiencing various issues, including chronic pain, substance abuse, and depression.
Each modality offers unique benefits, and the choice of therapy depends on factors such as the client’s specific symptoms, personal preferences, and the therapist’s expertise. Therapists may sometimes incorporate elements from multiple approaches to create a tailored treatment plan. Ultimately, all three therapies aim to improve mental health and well-being, providing individuals with the necessary tools to lead fulfilling lives.
Frequently Asked Questions

What are the key differences between CBT, DBT, and ACT?
CBT (Cognitive Behavioral Therapy) identifies and changes negative thought patterns and behaviors. It is structured and goal-oriented, emphasizing teaching clients coping skills and strategies for dealing with their problems.
DBT (Dialectical Behavior Therapy) is a form of CBT incorporating mindfulness and acceptance techniques. It addresses personality disorders, self-destructive behaviors, and emotional dysregulation. Clients learn to balance change and acceptance in their lives.
ACT (Acceptance and Commitment Therapy) promotes flexibility and values-based action. It emphasizes developing psychological flexibility, mindfulness, and connecting with personal values. Clients are taught to accept their thoughts and emotions while taking action in alignment with their values.
Which therapy is most effective for ADHD: DBT or CBT?
For ADHD, research tends to favor CBT. It teaches clients specific skills and strategies for managing their symptoms, such as time management, organization, and impulse control. DBT can also be helpful but is generally more focused on emotional regulation and interpersonal effectiveness.
Is DBT or CBT better suited for treating PTSD?
CBT, specifically Prolonged Exposure Therapy and Cognitive Processing Therapy, has strong evidence supporting its use in treating PTSD. These approaches help clients process traumatic memories, change negative thinking patterns, and develop coping strategies. DBT can be helpful for individuals with PTSD who also struggle with emotional dysregulation or self-destructive behaviors but might not specifically address the trauma itself.
How do CBT, DBT, and ACT compare for bipolar disorder?
CBT effectively manages bipolar disorder by helping clients identify and modify negative thought patterns, develop coping skills, and prevent relapse. DBT might be helpful for individuals with bipolar disorder who experience intense mood swings and impulsive behaviors, while ACT can help with emotional regulation and values-based action. The choice of therapy should be based on individual needs and preferences.
Does DBT integrate elements from both ACT and CBT?
DBT is primarily a form of CBT, but it does incorporate some elements of ACT, such as mindfulness and acceptance. However, DBT differs from ACT’s focus on dialectics (balancing change and acceptance) and emphasizes skills training for emotional regulation and interpersonal effectiveness.
How do the methods and goals of IFS differ from CBT and DBT?
IFS (Internal Family Systems) therapy focuses on the various “parts” within a person and their interactions. The goal is to create harmony amongst these parts and help clients develop new ways of relating to their emotions, thoughts, and behaviors. Unlike CBT and DBT, which are more structured and skills-based, IFS is centered around the concept of the “Self” and encourages self-awareness and a compassionate understanding of one’s internal world.
Jacob Maslow: A staunch advocate for mental health awareness, I take Escitalopram (Lexapro / Cippralex) to manage my challenges. Having undergone extensive therapy, I have firsthand experience with the transformative power of therapeutic modalities like DBT, CBT, and ACT. My journey is further shaped by navigating a difficult battle with an ex-partner suffering from severe narcissism, which has deeply affected my relationship with our children. Despite these hurdles, I find solace in long, introspective walks that help me center my thoughts. Through writing, I aim to illuminate the nuances of mental health and narcissism, offering hope and guidance to others in similar predicaments. My legal insights, shared on another platform, support those struggling with non-compliant partners and the complexities of co-parenting.
- 7 Ideas to Help You Relax and Unwind on a Family Vacation - April 27, 2025
- How Having Cybersecurity Protection Helps You Relax - April 25, 2025
- 8 Reasons Why Spending Time Outside Calms You Down - April 25, 2025
This site contains affiliate links to products. We will receive a commission for purchases made through these links.


 Exploring Different Therapies
Exploring Different Therapies Methods and Tools in Therapy
Methods and Tools in Therapy Understanding Therapy Effectiveness
Understanding Therapy Effectiveness
