As a BetterHelp affiliate, we receive compensation from BetterHelp if you purchase products or services through the links provided
Dialectical Behavior Therapy (DBT) and Acceptance and Commitment Therapy (ACT) are two distinct psychological interventions that have gained recognition for effectively addressing various mental health issues. Both therapies aim to improve emotional regulation and foster psychological flexibility to enhance overall well-being. However, they employ different techniques and philosophies to achieve these goals.
DBT, initially developed to treat borderline personality disorder, focuses on teaching skills that help individuals manage intense emotions, improve interpersonal relationships, and tolerate distress. On the other hand, ACT aims at promoting psychological flexibility by encouraging clients to recognize and accept their emotions, thoughts, and sensations while focusing on their values and committed actions towards valued living.
In comparing DBT and ACT, it is essential to consider their different approaches, effectiveness in treating mental health issues, coping strategies for behavioral concerns, and the use of specific modalities in group or individual therapy settings.
Key Takeaways
- DBT and ACT are distinct therapies, focusing on emotional regulation and psychological flexibility, respectively.
- Effectiveness varies depending on the mental health issue being treated and the individual’s needs.
- Both therapies can be adapted for group or individual settings, utilizing various techniques in clinical practice.
 Understanding Dialectical Behaviour Therapy (DBT)
Understanding Dialectical Behaviour Therapy (DBT)
Dialectical Behaviour Therapy (DBT) is a cognitive-behavioral therapy that focuses on helping individuals manage emotions, improve interpersonal relationships, and reduce self-destructive behaviors. It was initially developed to treat individuals with borderline personality disorder but has since been adapted to treat various mental health concerns.
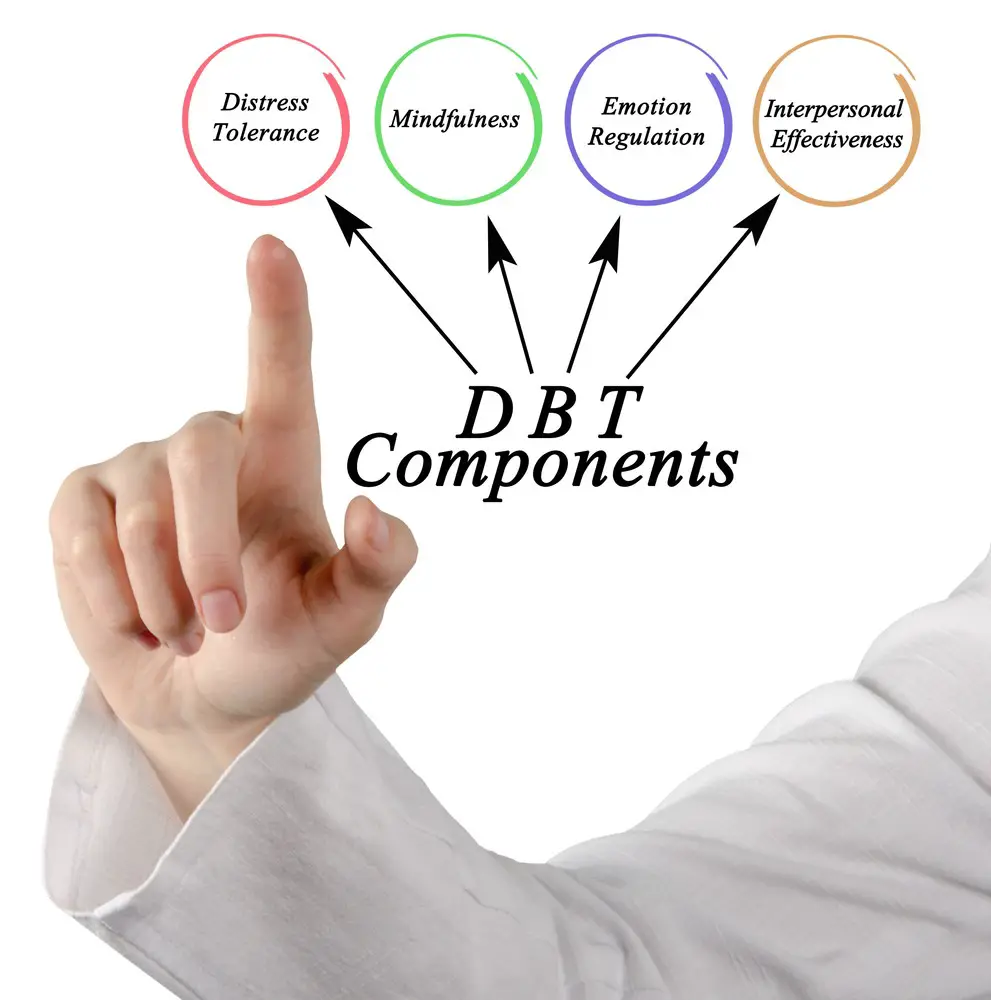
DBT is grounded in dialectics, emphasizing opposites’ balance and integration. This approach allows for the validation of a person’s emotional experiences while also encouraging behavior change. DBT consists of four main components: distress tolerance, emotion regulation, interpersonal effectiveness, and mindfulness.
Distress tolerance aims to help individuals learn how to cope with and survive difficult situations without resorting to self-destructive behaviors or emotional upheaval. This component teaches skills like distraction, self-soothing, and reality acceptance to help clients better navigate challenging emotions.
Emotion regulation focuses on identifying, labeling, and understanding emotions to reduce emotional intensity and increase control over emotional responses. This component includes techniques for changing negative emotional patterns and increasing the experience of positive emotions.
Interpersonal effectiveness targets the development of effective communication and relationship-building skills. These skills enable clients to assert their needs, set boundaries, and manage conflicts in a way that is respectful and collaborative. This component also explores the impact of one’s emotions on interpersonal situations and vice versa.
In addition to these three components, DBT incorporates mindfulness as a foundational practice. Mindfulness involves cultivating non-judgmental awareness of the present moment, allowing individuals to observe their emotions, thoughts, and behaviors without reacting impulsively. This increased self-awareness can lead to better decision-making and more effective emotion regulation.
DBT helps individuals develop a more balanced approach to their emotions and behaviors. By combining validation and behavior change strategies, clients are better equipped to navigate distressing situations and maintain healthy relationships.
 Understanding Acceptance and Commitment Therapy (ACT)
Understanding Acceptance and Commitment Therapy (ACT)
Acceptance and Commitment Therapy (ACT) is a unique approach to psychotherapy that emphasizes the importance of accepting situations and committing to personal values. This therapy model aims to increase psychological flexibility by helping individuals develop mindfulness skills and explore new ways of thinking.
ACT focuses on six core processes: acceptance, cognitive defusion, presence, self-awareness, values, and committed action. These processes help individuals recognize and manage their thoughts, emotions, and behaviors. In doing so, people can develop healthier coping strategies and engage in more fulfilling actions aligned with their values.
Mindfulness is a key component of ACT. It involves being present in the current moment and engaging with experience non-judgmentally. This practice allows individuals to become more aware of their thoughts and feelings, often providing a fresh perspective on challenging situations. This newfound awareness can lead to meaningful change.
A central concept in ACT is psychological flexibility, which refers to adapting to changing circumstances and pursuing valued goals despite challenging emotions or thoughts. Individuals learn to face their discomfort by targeting experiential avoidance rather than avoiding or suppressing it. This approach helps foster personal growth and resilience.
In summary, Acceptance, and Commitment Therapy is an innovative approach to mental health care that emphasizes acceptance, mindfulness, and commitment to personal values. It aims to enhance psychological flexibility, enabling individuals to create lasting change in their lives and overcome experiential avoidance.
 DBT and ACT: A Comparative Study
DBT and ACT: A Comparative Study
Dialectical Behavior Therapy (DBT) and Acceptance and Commitment Therapy (ACT) are both evidence-based approaches to psychotherapy that fall under the umbrella of cognitive behavioral therapy (CBT). Though they share some common goals and techniques, they differ in their focus, scope, and strategies to help clients overcome psychological difficulties.
DBT, developed by Dr. Marsha Linehan, was initially designed to treat individuals with borderline personality disorder. However, its efficacy has expanded to other conditions like depression, eating disorders, and addiction. The fundamental premise of DBT is the view that clients often struggle to balance opposing needs, desires, and beliefs. This therapy uses a combination of individual therapy, group skills training, and telephone consultations to teach clients skills in mindfulness, emotion regulation, interpersonal effectiveness, and distress tolerance.
On the other hand, ACT is a third-wave CBT approach created by Dr. Steven C. Hayes. It aims to help clients develop psychological flexibility and live under their values. ACT uses experiential, metaphorical, and linguistic techniques to achieve this goal. While not created for a specific disorder, ACT has proven effective in treating many conditions, including anxiety, depression, chronic pain, and substance abuse.
Both DBT and ACT employ mindfulness as a cornerstone in their treatment strategies. However, their usage of mindfulness may differ. In DBT, mindfulness is a skill amongst others, while in ACT, it is a process that fosters psychological flexibility. Additionally, DBT is structured in stages and targets specific problems through a defined hierarchy, whereas ACT remains flexible and adaptive in addressing client issues.
When examining the application of these therapies in a clinical setting, it is important to note that DBT requires an extensive commitment from both therapists and clients. It involves a comprehensive treatment plan, a team of therapists and usually lasts for at least one year. In contrast, ACT therapists can integrate the core principles into various other therapeutic approaches and adjust the length and intensity of treatment based on individual client needs.
In conclusion, although both DBT and ACT have their roots in CBT, these therapies differ in focus, methodology, and application. Both have demonstrated effectiveness in treating psychological difficulties, but the choice between them may depend on clients’ specific needs, therapists’ training and expertise, and the resources available for treatment.
 Effectiveness in Mental Health Issues
Effectiveness in Mental Health Issues
Dialectical Behavior Therapy (DBT) and Acceptance and Commitment Therapy (ACT) are well-known therapeutic approaches to treating various mental health issues. These therapies are effective in managing symptoms of several mental health conditions.
DBT, originally developed to treat borderline personality disorder, has shown impressive results for individuals struggling with other conditions such as depression, anxiety, bipolar disorder, and eating disorders. In DBT, clients are taught skills to regulate emotions, tolerate distress, improve relationships, and practice mindfulness, which can help address various mental health challenges.
For example, in cases of depression and anxiety, DBT helps clients identify and change negative thought patterns and learn strategies to cope with overwhelming emotions effectively. Similarly, for those with bipolar disorder, DBT provides the skills necessary to stabilize mood swings and minimize the impact of emotional triggers.
ACT, on the other hand, focuses on increasing psychological flexibility by helping clients accept their thoughts and emotions without judgment. This therapeutic approach has effectively treated various mental health disorders, including generalized anxiety disorder, obsessive-compulsive disorder, panic disorder, and various trauma-related conditions.
Through mindfulness and cognitive exercises, ACT encourages clients to develop a more accepting and compassionate relationship with their thoughts and feelings, which can significantly reduce distress and improve mental well-being. For example, individuals suffering from generalized anxiety disorder can benefit from ACT by learning to accept uncertainty and reduce self-defeating thought patterns.
Both DBT and ACT have shown promising results for people with eating disorders. While DBT emphasizes emotional regulation and interpersonal effectiveness, ACT focuses on accepting one’s thoughts and feelings to establish a healthier relationship with food and body image.
In summary, DBT and ACT have proven to be effective therapeutic approaches for a broad range of mental health issues, including depression, anxiety, trauma, bipolar disorder, eating disorders, and various other mental health conditions. These therapies can help individuals improve their overall mental health and well-being by addressing emotion regulation, distress tolerance, and psychological flexibility.
Coping with Behavioral Concerns
Coping with behavioral concerns is an essential aspect of mental health and well-being. Dialectical Behavior Therapy (DBT) and Acceptance and Commitment Therapy (ACT) are widely recognized therapies often employed in this domain. These two approaches share some similarities, such as incorporating mindfulness techniques, but they also differ.
DBT is a comprehensive, evidence-based therapy initially developed for individuals with borderline personality disorder. However, it has since been applied to various issues, including anger management, impulse control, and other behavioral challenges. DBT focuses on four key areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. Clients develop mindfulness skills to become more aware of their thoughts and emotions, which enables them to manage their behaviors more effectively. Additionally, clients learn to navigate their emotional responses to challenging situations through distress tolerance and emotion regulation skills.
In contrast, ACT is a process-oriented therapy that aims to help clients develop psychological flexibility. This therapy form encourages action that aligns with one’s values while accepting any accompanying unpleasant emotions. In recognizing that behavioral concerns often stem from a struggle to control feelings or thoughts, ACT encourages clients to develop coping strategies that align with their values rather than focusing on changing emotions directly.
When addressing behavioral concerns, it is essential to consider each client’s unique circumstances and needs. DBT and ACT offer effective tools to foster mindfulness and improve coping strategies. Clients may benefit from learning and applying DBT techniques, such as emotion regulation, to manage challenging emotions better, contributing to problematic behaviors. Meanwhile, using ACT principles can guide clients toward insightful, value-driven life choices that coincide with their personal goals. Consequently, each therapy offers a distinct pathway toward enhanced behavioral management rooted in mindfulness and self-awareness.
 Role in Treating Specific Disorders
Role in Treating Specific Disorders
Dialectical Behavior Therapy (DBT) and Acceptance and Commitment Therapy (ACT) are evidence-based treatments for various psychological disorders. While they share similarities, these therapies have distinct applications in treating specific disorders.
DBT is often used to treat individuals with borderline personality disorder (BPD), as it was initially developed for this population. However, DBT has also effectively treated other disorders, such as post-traumatic stress disorder (PTSD), substance abuse, and eating disorders. In DBT, clients learn skills in mindfulness, emotional regulation, distress tolerance, and interpersonal effectiveness, which enables them to manage symptoms, improve relationships, and enhance their overall quality of life.
Additionally, DBT has been used to address self-harm behaviors and suicidal ideation, which are prevalent in individuals with BPD and other mental health conditions. By teaching clients to identify and regulate emotions, DBT can reduce the likelihood of engaging in self-destructive behaviors.
On the other hand, ACT is a broader, more versatile approach that has been applied to various psychological disorders such as anxiety, depression, chronic pain, addiction, and even obsessive-compulsive disorder (OCD). In ACT, clients develop psychological flexibility through mindfulness, acceptance, and value-based actions, thus enabling better coping with emotions, thoughts, and behaviors related to their diagnosis.
For instance, ACT has been useful in treating panic disorder by helping individuals face anxiety-provoking situations willingly rather than attempting to avoid or eliminate panic symptoms. Similarly, ACT is applied to treat chronic pain by teaching clients to accept the presence of pain while engaging in meaningful activities aligned with personal values.
Both DBT and ACT have demonstrated benefits in substance abuse and addiction in helping individuals build healthier coping strategies and reduce the risk of relapse. While DBT focuses more on skill-building, ACT emphasizes developing psychological flexibility to accept cravings and urges without acting on them, thus promoting long-term recovery.
In conclusion, DBT and ACT have valuable roles in treating various psychological disorders. Each therapy provides unique tools and strategies tailored to specific diagnoses, enabling clients to experience improved mental health and well-being.
 Treatment Modalities: Group or Individual Therapy
Treatment Modalities: Group or Individual Therapy
Dialectical Behavior Therapy (DBT) and Acceptance and Commitment Therapy (ACT) offer various treatment modalities to address different individual needs, especially in group or individual therapy. While individual therapy within these approaches emphasizes personal progress and tailored interventions, group settings help participants to learn and practice various skills in a supportive environment.
In DBT, group skills training is essential to the therapy process. Clients attend weekly sessions to learn and practice vital coping strategies related to mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness. These group sessions, led by a trained therapist, offer a safe and nurturing space for individuals to share their experiences, gain peer support, and receive valuable feedback. The collaborative environment of the group setting encourages participants to relate to others’ experiences and allows for normalizing their emotions and thoughts.
ACT, on the other hand, focuses more on individualizing therapy sessions to address unique psychological experiences and target problematic behavior patterns. Clients typically engage in one-on-one talk therapy or psychotherapy sessions with a trained therapist to navigate their emotional experiences and commit to desired behavioral changes. Some ACT practitioners may also offer group therapy sessions to complement individual treatment. By utilizing mindfulness and acceptance strategies, participants learn techniques to develop psychological flexibility and stress resilience in these group settings.
Both group and individual therapy sessions in DBT and ACT exhibit unique benefits that cater to specific needs within their therapeutic approaches. While group skills training in DBT helps provide a sense of community and offers extensive learning opportunities, individual therapy in ACT allows for personalized guidance and focused attention on the client’s emotional and behavioral challenges. Consequently, the choice between group or individual therapy sessions depends on the client’s preferences, therapeutic needs, and the therapist’s assessment and recommendation.

DBT and ACT Techniques in Clinical Practice
Dialectical Behavior Therapy (DBT) and Acceptance and Commitment Therapy (ACT) are powerful therapeutic approaches used in clinical practice. Both therapies focus on helping clients develop effective coping strategies and skills for managing and accepting their emotional experiences. While DBT and ACT have some commonalities, key differences exist in their methodologies and techniques.
DBT is an evidence-based therapy rooted in traditional cognitive-behavioral therapy (CBT) principles. It specifically targets individuals with borderline personality disorder (BPD) but has also been adapted for other mental health disorders. Therapy sessions typically focus on fostering mindfulness skills, emotion regulation, interpersonal effectiveness, and distress tolerance. In DBT, therapists often provide phone coaching outside of therapy sessions to support clients in applying coping strategies learned during therapy.
ACT, on the other hand, is a mindfulness-based therapeutic approach that assists clients in dealing with difficult emotions and thoughts by encouraging psychological flexibility. This approach emphasizes directing attention to the present moment, openly accepting difficult feelings and thoughts, and acting congruently with one’s values. ACT focuses on six core processes: acceptance, defusion, self-as-context, contact with the present moment, values, and committed action.
Both therapies emphasize mindfulness skills to help clients gain greater awareness and control over their thoughts, feelings, and behaviors. While DBT focuses on teaching clients specific coping strategies and skills to manage their emotions, ACT strives to foster a healthy relationship with thoughts and feelings through acceptance and psychological flexibility.
In clinical practice, therapists choose between DBT and ACT based on clients’ concerns and treatment goals. Both therapies are well-suited to address psychological challenges like emotion dysregulation, anxiety, depression, and trauma-related disorders. In any case, selecting a therapeutic approach relies heavily upon the therapist’s expertise, training, and understanding of the client’s needs.
Conclusion
DBT and ACT are both evidence-based therapies that have shown efficacy in treating various mental health issues. Their approach and goals differ, with DBT focusing on skills training and emotional regulation, while ACT emphasizes psychological flexibility and accepting thoughts and feelings without judgment.
Both therapies can enable individuals to make lasting changes in their lives as they provide tools for managing emotions, behaviors, and thoughts. The choice of therapy depends on the individual’s needs and preferences and the specific mental health concern being addressed. Consulting with a mental health professional can help determine the most suitable approach for each person.
In summary, this article has provided information on the key differences between DBT and ACT, two prominent therapeutic approaches used in mental health treatment. It is essential to consider each therapy’s unique characteristics and goals to decide on the best course of action for one’s mental well-being.
Frequently Asked Questions

What are the main differences between DBT and ACT therapy?
DBT (Dialectical Behavior Therapy) and ACT (Acceptance and Commitment Therapy) are evidence-based therapies that help individuals cope with challenging emotions and thoughts. DBT primarily focuses on individuals with borderline personality disorder (BPD) and emphasizes skills development in four areas: emotion regulation, distress tolerance, mindfulness, and interpersonal effectiveness. ACT, on the other hand, aims to help individuals accept their thoughts and feelings while committing to values-based actions applicable to a broader range of mental health conditions.
How do DBT and ACT compare in treating OCD?
Both DBT and ACT can help treat Obsessive-Compulsive Disorder (OCD). While DBT may be useful in teaching patients skills to tolerate anxiety and distress, ACT focuses on assisting patients in accepting their compulsive thoughts and redirecting their actions towards personal values. In some cases, clinicians may combine both treatments for more effective outcomes.
Can DBT and ACT be effectively combined in treatment?
Combining DBT and ACT can be effective in treatment as both therapies emphasize mindfulness and acceptance. This dual approach can help individuals develop useful skills for managing emotions and enhancing their overall quality of life. However, the specific treatment plan depends on the individual’s unique needs and goals and their clinician’s expertise.
How does radical acceptance in DBT differ from acceptance in ACT?
Radical acceptance in DBT involves fully embracing and accepting the present moment, including all its challenges, without attempting to change it. This is a key component of distress tolerance in DBT. In ACT, acceptance refers to the willingness to experience uncomfortable thoughts and feelings without engaging in avoidance behaviors. Both approaches share similarities but serve different purposes in their respective therapies.
What are the key components of DBT and ACT therapies?
The key components of DBT include mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness. These components aim to provide patients with skills to manage their emotions, tolerate distress, and navigate relationships effectively.
The key components of ACT include acceptance, cognitive defusion, mindfulness, values, committed action, and self-as-context. These core principles allow patients to embrace their thoughts and emotions while focusing on meaningful actions aligned with their values.
Why has DBT faced criticism and how does it compare to ACT?
DBT has faced criticism for being overly complex and time-consuming compared to other therapies. The extensive focus on skills development, which requires a significant commitment from the patient and the therapist, may not be a suitable fit for everyone. However, DBT is considered an effective treatment for borderline personality disorder and has shown positive results for other mental health conditions.
ACT is more flexible and perhaps easier to implement across different patient populations. ACT focuses on helping individuals accept their thoughts without judgment and align their actions with their values. While both therapies share components like mindfulness and acceptance, the choice between the two depends on an individual’s unique needs, goals, and therapeutic preferences.
Jacob Maslow is a fervent advocate for mental health, drawing from personal experiences that have deeply shaped his understanding of therapeutic approaches like DBT and ACT. A therapy veteran, Jacob relies on Lexapro and the calming ritual of daily long walks to navigate a tumultuous journey with an ex-spouse displaying strong narcissistic tendencies. This experience, marked by court disputes and estrangement from his children, underscores the critical importance of understanding and managing mental health challenges. Jacob pens insightful articles delving into therapies, mental health, and the dark shadows of narcissism. With a hope to be a beacon for others, his writings emphasize that conquering mental health hurdles is attainable. Jacob’s legal platform also supports those wrestling with non-compliant spouses and the complexities of co-parenting.
- How Having Cybersecurity Protection Helps You Relax - April 25, 2025
- 8 Reasons Why Spending Time Outside Calms You Down - April 25, 2025
- 5 Helpful Ideas for Managing Stress During a Plumbing Emergency - April 24, 2025
This site contains affiliate links to products. We will receive a commission for purchases made through these links.


 Understanding Dialectical Behaviour Therapy (DBT)
Understanding Dialectical Behaviour Therapy (DBT) Understanding Acceptance and Commitment Therapy (ACT)
Understanding Acceptance and Commitment Therapy (ACT)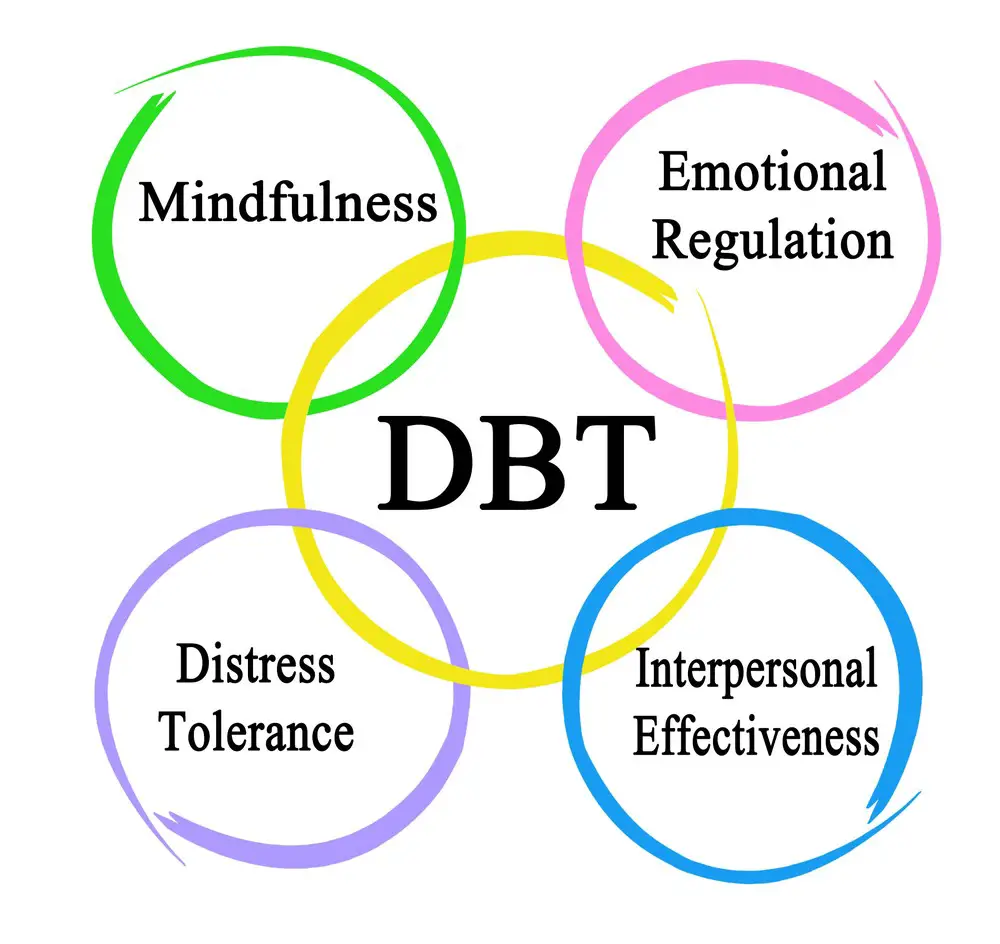 DBT and ACT: A Comparative Study
DBT and ACT: A Comparative Study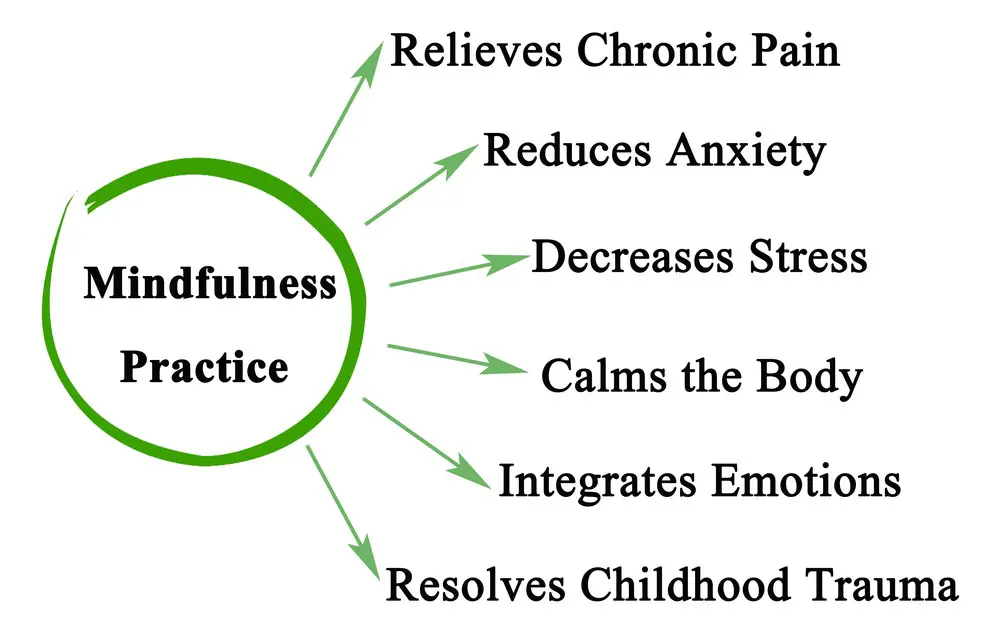 Effectiveness in Mental Health Issues
Effectiveness in Mental Health Issues Role in Treating Specific Disorders
Role in Treating Specific Disorders Treatment Modalities: Group or Individual Therapy
Treatment Modalities: Group or Individual Therapy
