As a BetterHelp affiliate, we receive compensation from BetterHelp if you purchase products or services through the links provided
Stress is a common factor in our daily lives, influencing physical and mental health. But can stress cause diverticulitis, a digestive disorder characterized by inflammation or infection in small pouches that form in the lining of the colon? That is the question we seek to explore in this article.
Diverticulitis is a condition that affects millions of people worldwide. While experts agree that its primary cause is a low-fiber diet, stress may play a role in its development or exacerbation. Understanding the link between stress and diverticulitis can help in proactive prevention, early detection, and management of this painful disorder.
Key Takeaways
- A low-fiber diet primarily causes diverticulitis, but stress may contribute to its development.
- Early detection and management are essential to prevent complications
- A balanced diet, stress reduction, and exercise can minimize the risk of developing diverticulitis
 Understanding Diverticulitis
Understanding Diverticulitis
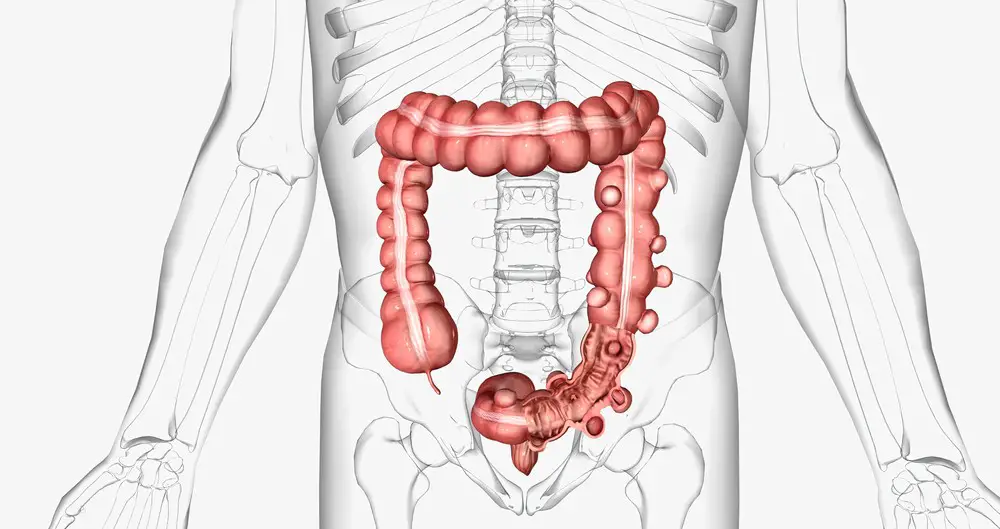
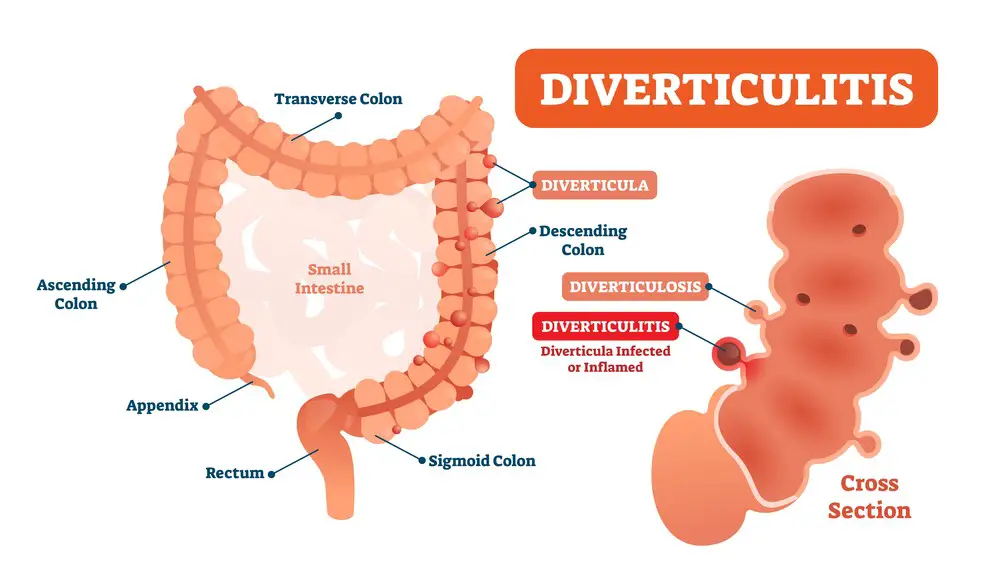
Diverticulitis is a condition that affects your digestive system, specifically the colon or large intestine. It occurs when small pouches called diverticula, which can form in the walls of your digestive tract, become inflamed or infected. Let’s dive deeper into what causes this condition, its symptoms, and how it relates to stress.
The development of diverticula, or these small pouches, is usually a result of age and lifestyle factors, such as low-fiber diets and lack of exercise. As you grow older, the walls of your colon can weaken, allowing the formation of diverticula. Once these pouches develop, bacteria or trapped stool can lead to inflammation of these diverticula, causing diverticulitis. Symptoms of this condition can range from abdominal pain and fever to more severe complications like abscesses or even perforations in the intestine.
Now, you may be wondering how stress can contribute to diverticulitis. While stress in itself may not directly cause diverticulitis, it can play a role in exacerbating the inflammation. High-stress levels can negatively affect your immune system, making it harder for your body to fight off bacterial infections within the inflamed diverticula. Furthermore, stress can also lead to unhealthy lifestyle habits, such as poor diet choices and lack of exercise, thus increasing the risk of developing diverticula in the first place.
To sum it up, while stress might not directly cause diverticulitis, it can be a contributing factor that worsens the condition. Paying attention to your lifestyle habits and overall stress management can benefit your colon health and well-being.
 Cause and Effect: Stress and Diverticulitis
Cause and Effect: Stress and Diverticulitis
Stress is something that inevitably affects your life at one point or another. Understanding stress’s impact on your health is important, particularly concerning diverticulitis. While there may not be a direct link between stress and diverticulitis, stress can indirectly influence this condition.
Diverticulitis is a digestive disorder characterized by inflammation and infection in your intestinal pouches called diverticula. These pouches can form when you experience weak spots in the colon wall and prolonged straining during bowel movements.
Now, you might be wondering how stress can contribute to diverticulitis. Well, stress affects the brain, which in turn influences numerous body functions. It can weaken your immune system, making it less efficient in fighting off harmful bacteria. This is especially concerning in diverticula, as these pouches can easily harbor bacteria, leading to infection.
Additionally, stress can cause disruptions in your bowel habits. You might experience changes in the frequency or consistency of bowel movements, which can contribute to the development of diverticula. These changes may also lead to constipation, forcing you to strain during bowel movements and adding more strain on your colon.
Furthermore, stress can alter your gut’s balance of good and bad bacteria. This shift can result in an overgrowth of harmful bacteria, which may lead to inflammation and infection in the diverticula.
In summary, while stress is not a direct cause of diverticulitis, it can indirectly pave the way for this condition by affecting your gut health, immune response, and bowel control. By managing your stress levels, you can better protect yourself from the development and recurrence of diverticulitis.

Recognizing Diverticulitis Symptoms
When dealing with stress, it’s important to be aware of its potential impact on various aspects of your health, including the possibility of developing diverticulitis. To help you recognize the signs and symptoms of this condition, pay attention to some of the common indicators described below.
One of the first symptoms you might experience is pain in the abdomen, usually on the lower left side. This pain can range from mild to severe and may occur suddenly or gradually over a few days. If you’re noticing persistent abdominal pain, don’t ignore it—it could be a sign of diverticulitis.
Along with the abdominal pain, you might also experience nausea or vomiting. These symptoms might make it difficult for you to maintain an appetite, and you might lose weight unintentionally. Be sure to monitor any sudden changes in your eating habits or feelings of nausea, as they could be connected to diverticulitis.
Another common symptom is a change in bowel habits. This could be in the form of diarrhea or constipation. It may also include a feeling of incomplete bowel movements or the constant urge to have a bowel movement.
In some cases, people with diverticulitis may experience rectal bleeding. This could be in bright red blood on the toilet paper or in the toilet bowl. While not always a sign of diverticulitis, rectal bleeding should be addressed with a healthcare professional to determine the cause and initiate appropriate treatment.
In addition to these symptoms, you might notice abdominal tenderness or bloating. In many cases, these symptoms can worsen after eating a meal, so keep track of your diet and how it affects your abdominal pain and discomfort.
In summary, if you’re experiencing any combination of these symptoms—abdominal pain, nausea, vomiting, diarrhea, constipation, tenderness, rectal bleeding, or bloating—it’s essential to consult a healthcare professional. Identifying and treating diverticulitis early can reduce the risk of complications and alleviate your digestive discomfort.
Complications of Diverticulitis
Diverticulitis can cause various complications, making it crucial for you to be aware of them. Knowing these potential challenges can help you take the necessary steps to prevent them or consult your doctor promptly.
Abscess formation is a common complication when the inflamed diverticula becomes infected. Bacteria from your digestive system can invade and cause a collection of pus in the affected area. If left untreated, an abscess may require draining or surgical intervention to prevent it from spreading further.
In some cases, diverticulitis can lead to a fistula. A fistula forms when the inflamed diverticula penetrates through the walls of the intestine, creating an abnormal connection between the bowel and other organs. This can lead to bacterial infection and inflammation in other parts of your body.
One potentially severe complication is peritonitis when the inflamed diverticula rupture and release bacteria into the abdominal cavity. Peritonitis is a medical emergency that requires immediate treatment, often involving surgery and potent antibiotics, as it can cause life-threatening consequences if left untreated.
With acute diverticulitis, scarring of the colon may occur over time due to recurrent inflammation. This can result in a narrowed colon area, making it challenging for stool to pass and potentially causing a blockage.
Lastly, perforation of the colon is another possible complication. This occurs when the inflamed diverticula creates a hole in your colon, allowing bacteria and digestive waste to leak into the surrounding area. This situation can be dangerous, putting you at risk for an abdominal infection or sepsis.
In summary, complications of diverticulitis can range from abscesses to potentially life-threatening conditions like peritonitis. You must monitor your symptoms closely and consult your healthcare professional if you’re concerned about any of these complications. Your doctor can guide you through appropriate treatment and care, ensuring the best possible outcome for your health.
Diverticulitis Diagnosis
When you suspect you may suffer from diverticulitis, your doctor will conduct several tests to diagnose accurately. It’s essential to get a precise diagnosis to help determine the best course of treatment for your condition.
The first step in a diverticulitis diagnosis is usually a thorough discussion of your symptoms and medical history with your doctor. They may also physically examine your abdomen to check for tenderness or swelling.
To further investigate your situation, your doctor may request several tests, including:
- Blood tests: These help identify if there’s an infection or inflammation in your body. Elevated white blood cell counts could indicate an issue related to diverticulitis.
- Stool test: By examining your stool, your doctor can rule out other potential causes of your symptoms, such as bacterial infections or parasites.
Imaging tests can provide a more in-depth look into your colon and surrounding organs, allowing for a more accurate diagnosis. Several imaging tests can help identify diverticulitis, such as:
- Colonoscopy: This procedure involves inserting a thin, flexible tube with a tiny camera at the end (colonoscope) into your rectum to examine the inside of your colon. A colonoscopy can help reveal diverticula and assess the severity of your condition.
- CT scan: A computerized tomography (CT) scan uses X-rays to create detailed pictures of your abdomen. In cases of suspected diverticulitis, a CT scan can be beneficial in detecting inflammation, abscesses, or other complications.
Once your doctor has analyzed the results of these tests, they can more accurately determine if you have diverticulitis and recommend an appropriate treatment plan. Remember that early diagnosis is crucial in addressing your symptoms and preventing severe complications. Should you notice any signs of diverticulitis, consult your doctor immediately.
Treatment for Diverticulitis
When dealing with diverticulitis, knowing the various treatment options available to manage the condition effectively is essential. The severity of your symptoms and the extent of inflammation in your colon will determine the appropriate course of action. Here are some treatment options that can help you manage diverticulitis:
1. Antibiotics
One of the first steps in treating mild diverticulitis is taking antibiotics prescribed by your doctor. These medications target the infection and inflammation in your colon, helping to reduce your symptoms and allowing your colon to heal.
2. Clear liquid diet
While recovering from diverticulitis, your doctor may advise you to follow a clear, liquid diet for a short period. This temporary diet allows your digestive system to rest and heal, reducing the strain on your inflamed colon. Some examples of clear liquids that you can consume include:
- Water
- Broth
- Ice pops
- Gelatin
- Clear fruit juices with no pulp
3. Pain medications
Your doctor may recommend pain medications for managing the discomfort associated with diverticulitis. Always follow their advice for the appropriate medication and dosage.
4. Hospitalization
Sometimes, diverticulitis may cause severe symptoms or complications that require hospitalization. In these instances, you will receive intravenous antibiotics and fluids to help manage your infection and support your recovery.
5. Surgery
Surgery could be viable if your diverticulitis doesn’t respond well to conservative treatments or you have multiple severe episodes. There are two primary surgical approaches for diverticulitis:
- Primary bowel resection: In this procedure, the affected section of the colon is removed, and the remaining parts are reconnected. This surgery allows your intestinal system to return to normal after healing.
- Bowel resection with colostomy: In more severe cases, your surgeon may create a temporary or permanent colostomy. This involves diverting a portion of the colon through an opening in your abdominal wall, allowing waste to exit your body through a special pouch.
By familiarizing yourself with these treatment options, you can work with your healthcare team to find the best approach for managing your diverticulitis and regaining control over your health.
 Preventing Diverticulitis
Preventing Diverticulitis
Managing stress is vital to keep your digestive system healthy and prevent diverticulitis. One of the keys to doing so is to follow a well-balanced diet, which includes the right amount of fiber, nutrition, and fluids. In addition to a healthy diet, regular exercise can also play a significant role in keeping stress at bay and promoting gut health. This section will discuss the various ways you can help prevent diverticulitis.
Fiber-Rich Foods
Consuming a fiber-rich diet can greatly contribute to the prevention of diverticulitis. A fiber-rich diet includes plenty of fruits, vegetables, and whole grains. By adding fiber to your meals, you are not only promoting regular bowel movements but also helping to reduce pressure within your digestive system. Some examples of fiber-rich foods are:
- Fruits: Apples, pears, strawberries, raspberries
- Vegetables: Broccoli, spinach, sweet potatoes, carrots
- Whole grains: Brown rice, quinoa, whole wheat bread, whole grain pasta
Nutrition and Hydration
A balanced diet focused on essential nutrients is crucial to maintaining a healthy digestive system. This includes consuming enough vitamins, minerals, and protein, which can be found in lean meats, nuts, and seeds. In addition to proper nutrition, staying hydrated by drinking adequate water or other fluids is essential for preventing constipation and keeping your digestive system functioning efficiently.
Exercise Regularly
Regular physical activity can help reduce stress and promote good health, including a healthy digestive system. Exercise helps improve circulation, aids in digestion, and supports regular bowel movements. Incorporate activities like walking, cycling, swimming, or yoga into your daily routine to keep your body in optimal condition.
Adopt a stress Management Technique
Stress can be a silent trigger for diverticulitis, so practicing stress management techniques is important to ensure your digestive health remains in check. Some effective practices for stress management include mindfulness meditation, deep breathing exercises, or engaging in a hobby you enjoy.
In summary, the key to preventing diverticulitis is to adopt a fiber-rich and well-balanced diet, stay properly hydrated, and integrate regular exercise into your daily routine. Don’t forget to include stress management techniques to keep your digestive system in peak condition. By following these recommendations, you’re well on your way to maintaining a healthier and happier gut.
Risk Factors for Diverticulitis
Many factors contribute to the development of diverticulitis, and some of these risk factors might already be a part of your lifestyle. Understanding them can help you take steps to minimize your risk. Here are the most common risk factors to be aware of:
Age: As you grow older, your risk of developing diverticulitis increases. It is more common among people who are over the age of 40, and the likelihood keeps rising as you age.
Obesity: Being overweight or obese isn’t just bad for your heart and joints; it can also put you at a higher risk for diverticulitis. The extra weight can increase pressure on your colon, making the formation of diverticula more likely.
Smoking: If you’re a smoker, quitting can do wonders for your overall health, but it may also help reduce your risk of diverticulitis. Smoking weakens your immune system, interferes with blood flow, and can contribute to inflammation, making it harder for your body to heal and fight infections.
Genetics: Your family history can affect your risk of developing diverticulitis. If your close relatives have had this condition, you may also be more likely to develop it.
Health conditions: Certain health conditions, such as diabetes, autoimmune disorders, and chronic kidney disease, can increase risk. These conditions compromise your immune system, making it easier for infections to take hold.
To reduce your risk, consider:
- Eating a high-fiber diet to help maintain bowel regularity and prevent constipation.
- Engaging in regular physical activity to promote healthy bowel function.
- Drinking plenty of water to stay hydrated and help with digestion.
- Reducing stress levels, as stress may contribute to inflammation in the colon.
Remember that managing your overall health is essential in preventing diverticulitis and other medical problems. Stay mindful of these risk factors and make positive changes in your lifestyle to protect yourself.
 Warning Bells: Signs You Might Need Therapy for Stress
Warning Bells: Signs You Might Need Therapy for Stress
Ever feel like you’re carrying the world’s weight on your shoulders? Stress has a sneaky way of seeping into the corners of our lives, making us more susceptible to health issues like diverticulitis. Here are some signs that stress is becoming an unwelcome tenant in your life:
- Chronic Fatigue: You’re always tired, no matter how much sleep you get.
- Heightened Irritability: You snap more often than a turtle with an attitude.
- Persistent Anxiety: The dread of impending doom never really leaves you.
- Mood Swings: You go from ecstatic to devastated faster than a roller coaster ride.
- Unexplained Aches and Pains: Your body starts to rebel, manifesting stress physically.
Tip: Listen to your body. If you recognize more than one of these symptoms, it might be time to consult a mental health professional.
Mapping the Mind: Goals of Stress Therapy
Once you decide to seek help, what can you expect? Let’s lay down some groundwork for the mission ahead:
- Unearth the Roots: Understand the root causes of your stress.
- Equip Yourself: Learn coping mechanisms to deal with triggering situations.
- The Balance Beam: Work on achieving a healthy work-life balance.
- Build Resilience: Gain emotional strength to bounce back from setbacks.
- Mindful Living: Embrace mindfulness as a lifestyle, not just a technique.
Milestones and Checkpoints: Tracking Your Progress in Therapy
Progress in therapy isn’t always linear, but that doesn’t mean it’s not happening. Here’s how you can track your progress:
- Bi-weekly Check-ins: Have short reflections every two weeks to gauge how you feel compared to when you started.
- Skillset Growth: Notice if the coping skills you’ve learned in therapy make stressful situations easier to handle.
- Emotional Articulation: If you find it easier to articulate your feelings, you’re definitely on the right path.
- Improved Relationships: As you manage your stress, note if your interpersonal relationships flourish.
- Happiness Index: Lastly, are you generally happier and more content?
List Format for Milestones:
- Bi-weekly check-ins
- Skillset growth
- Emotional articulation
- Improved relationships
- Happiness index
Remember, therapy isn’t a sign of weakness; it’s a stepping stone toward a healthier, more balanced life. By keeping track of your therapy goals and progress, you’re not just finding a way to manage stress and its potential impact on conditions like diverticulitis; you’re mapping out a journey to a more peaceful, balanced life.
Conclusion
In summary, stress can indeed contribute to diverticulitis. It’s important to remember that while stress is not the sole cause of this condition, it can aggravate or exacerbate its symptoms. By managing stress levels and adopting a healthy lifestyle, you can effectively reduce your risk of developing diverticulitis or lessen its impact if you already have the condition.
- Managing stress: Consider incorporating stress-reduction techniques such as mindfulness, meditation, yoga, or deep breathing exercises into your daily routine. Seek professional help, and try to identify and avoid common stressors.
- Healthy lifestyle: Adopting a balanced, fiber-rich diet can greatly reduce your risk of developing diverticulosis and diverticulitis. Stay well-hydrated, exercise regularly, and maintain a healthy weight to decrease your risk.
- Stay informed: Stay up-to-date with the latest research and findings about diverticulitis and its potential causes, including the role of stress. This will enable you to make informed decisions about your healthcare and lifestyle choices.
By following these tips, you’ll be well on your way to managing stress and keeping diverticulitis at bay. Remember, it’s essential to prioritize self-care, listen to your body, and consult with a healthcare professional before making any drastic changes to your behavior or diet.
Frequently Asked Questions

How does stress affect diverticulitis?
Stress can indirectly affect diverticulitis by altering the way your body functions. When you’re under stress, your body releases stress hormones, which can cause inflammation in the digestive system, potentially exacerbating diverticulitis symptoms. Additionally, stress may lead to unhealthy coping mechanisms, including overeating or not eating enough, which can affect your gut health.
What role does anxiety play in diverticulitis flare-ups?
Anxiety is a form of emotional stress, and like other forms of stress, it can contribute to diverticulitis flare-ups. Anxiety can cause the release of stress hormones, leading to inflammation in the digestive system. It can also make you more sensitive to pain, making symptoms of diverticulitis feel even more intense. Moreover, anxiety may lead to changes in your eating habits, further affecting gut health.
Can emotional stress lead to diverticulitis symptoms?
Yes, emotional stress can potentially lead to diverticulitis symptoms. Emotional stress, like physical stress, triggers the release of stress hormones, which can cause inflammation in the digestive system and exacerbate symptoms of diverticulitis. Emotional stress might also lead to unhealthy coping habits, such as overeating, binge eating, or eating too little, affecting your gut’s health and function.
Is there a connection between stress and diverticulitis flare-ups?
There appears to be a connection between stress and diverticulitis flare-ups. Stress not only causes an increase in inflammation due to the release of stress hormones, but it can also lead to changes in eating habits and other lifestyle factors, which can affect gut health. By managing stress, you might minimize the risk of diverticulitis flare-ups.
How can I manage stress to prevent diverticulitis episodes?
To manage stress and prevent diverticulitis episodes, consider implementing some of the following strategies:
- Practice relaxation techniques like deep breathing exercises, meditation, or yoga.
- Exercise regularly, aiming for at least 30 minutes of moderate activity most days of the week.
- Maintain a balanced diet rich in fiber and low in inflammatory foods.
- Prioritize sleep, aiming for 7-9 hours per night.
- Seek social support from friends, family, or support groups.
- Consider talking to a mental health professional, such as a therapist or counselor, for additional guidance and support.
What lifestyle changes can reduce stress-induced diverticulitis?
Several lifestyle changes can help reduce the risk of stress-induced diverticulitis:
- Adopt stress management techniques like meditation, deep breathing exercises, or mindfulness.
- Maintain a regular exercise routine.
- Make dietary changes to increase fiber intake and minimize inflammatory foods.
- Prioritize sleep and establish a consistent sleep schedule.
- Nurture social connections and seek support from loved ones.
- Seek professional help if needed, such as therapy or counseling.

About the Author: Jacob Maslow—A Journey from Tragedy to Advocacy ??
I’m Jacob Maslow, and if there’s one thing life has taught me, resilience is more than just a buzzword—it’s a necessity. ?️ My life story has its fair share of dramatic twists. I survived the 9-11 attacks ??; I worked on the 101st floor and lost over a thousand colleagues on that dreadful day. This painful experience was a turning point that shifted my career toward working from home. ???
During this period, I shouldered caring for our kids ?? while my then-wife worked full-time, often through the night ?.
After our separation, our children adapted to living in two households ??, maintaining a close relationship with both parents. That is, until last year, when my ex-wife decided to sever all communication between me and our children. ? Now, I live alone in a three-bedroom apartment, the emptiness of the two unused bedrooms weighing heavily on me each day. ?️
To manage the emotional and psychological burden ?, I have turned to BetterHelp—an online therapy service I use and highly recommend. ?⚕️?⚕️ I am a therapy veteran and take Lexapro to manage my mental health issues. ? BetterHelp has been instrumental in helping me cope with the nightmarish reality of my kids being unjustly taken away from me. ?️
My ex-wife suffers from severe narcissism ?, which has only intensified over the years. This has led her to engage in reckless behaviors like affairs with community leaders, followed by vindictive smear campaigns—classic traits of narcissistic personality disorder. ? Despite court orders, she has continued to breach our shared custody arrangements ??, and the legal battle remains ongoing ⚖️.
I take long, soul-searching walks every day ?♂️ to clear my head and gain perspective. Through writing articles like this ?, I aim to help others facing mental health challenges or dealing with a narcissistic partner. My advocacy extends to a legal website ? dedicated to helping individuals battling spouses who weaponize children instead of responsibly co-parenting. ?????
The struggle with my ex-wife and the separation from my children have been harrowing for my mental health ?. But I believe that anyone can conquer their mental health issues ?, as I am learning to do every day. Thank you for reading ?, and I hope my insights can provide some comfort or guidance ?.
- 3 Ways Wearing a Hat Can Help Lower Your Stress Levels - April 19, 2025
- Breaking the Silence: Why Men’s Mental Health Matters More Than Ever - April 15, 2025
- How to Transform a Home’s Patio Space into a Relaxing Space - March 23, 2025
This site contains affiliate links to products. We will receive a commission for purchases made through these links.

 Understanding Diverticulitis
Understanding Diverticulitis Cause and Effect: Stress and Diverticulitis
Cause and Effect: Stress and Diverticulitis Preventing Diverticulitis
Preventing Diverticulitis Warning Bells: Signs You Might Need Therapy for Stress
Warning Bells: Signs You Might Need Therapy for Stress