As a BetterHelp affiliate, we receive compensation from BetterHelp if you purchase products or services through the links provided
Borderline Personality Disorder (BPD) is a complex mental health condition characterized by intense emotions, difficulty in maintaining stable relationships, and a distorted sense of self. One lesser-known behavior often observed in individuals with BPD is “mirroring.” This is when a person unintentionally imitates the emotions, behaviors, or attitudes of those they interact with, sometimes to the point of losing their identity. While mirroring can be a natural part of human interaction, it becomes more pronounced and persistent within the context of BPD.
Understanding mirroring entails recognizing that individuals with BPD may use this behavior as a strategy, albeit unconsciously, to connect with others. This can stem from an underlying fear of rejection or abandonment, leading to efforts to align themselves closely with those around them. It not only serves to establish a sense of connection but also to gain a feeling of control in social situations, which can be particularly challenging for those with the disorder.
Treatment and support for coping with BPD and its associated behaviors, like mirroring, involve a multi-faceted approach. Therapy often plays a central role, including Dialectical Behavior Therapy (DBT), which helps individuals develop skills to manage emotions and improve relationships. Support networks and educational resources also provide crucial backup for those looking to understand and manage symptoms of BPD.
Key Takeaways
- Mirroring in BPD is a coping mechanism tied to a distorted self-image and fear of abandonment.
- This behavior is often an unconscious attempt to connect and gain control in social settings.
- Managing BPD and mirroring involves therapy, skills development, and supportive resources.
 Understanding BPD
Understanding BPD
Borderline Personality Disorder (BPD) is a complex mental illness marked by unstable moods, behaviors, and relationships. In this section, you’ll gain insight into its core characteristics, how it’s diagnosed, and particular aspects like mirroring and attachment styles.
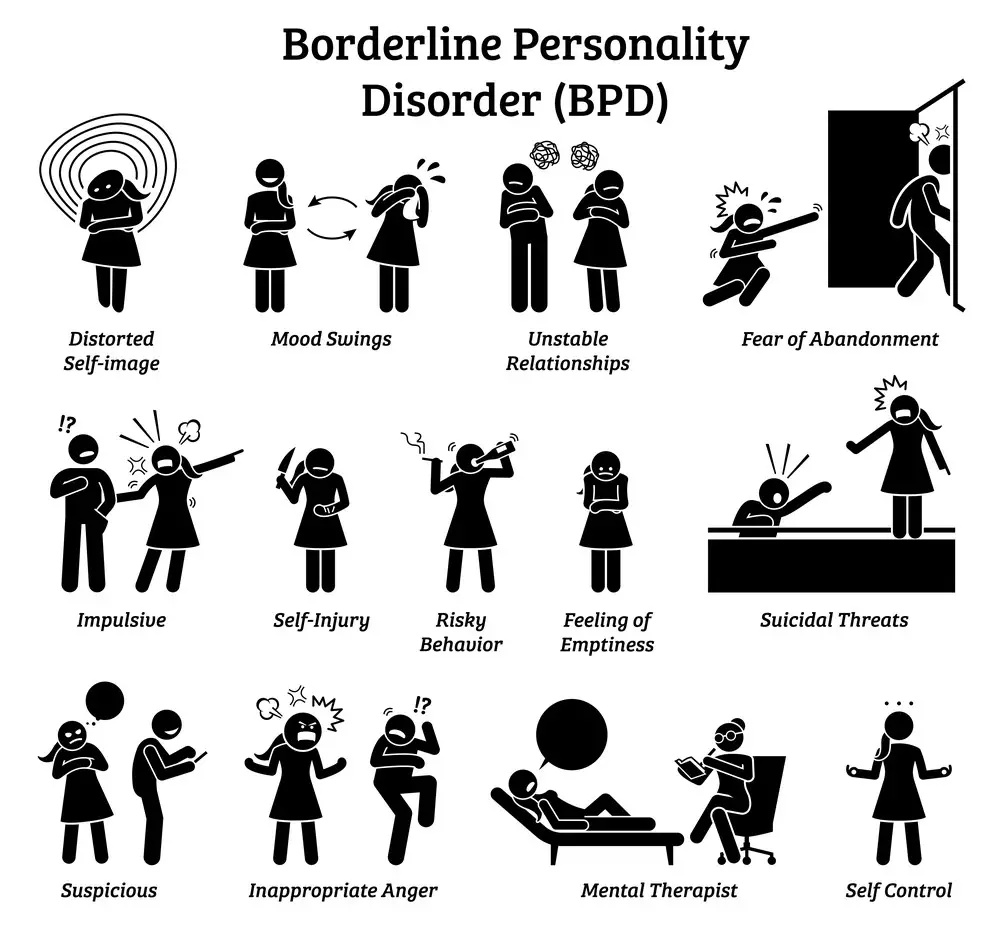
Core Characteristics of BPD
BPD manifests through a variety of symptoms that significantly impair one’s life. Emotional instability is a hallmark, with feelings that rapidly fluctuate and can seem overwhelming. Individuals may also experience intense episodes of anger, depression, and anxiety. Impulsive behaviors, like spending sprees or reckless driving, can be a coping mechanism to manage emotional turmoil.
- Key Takeaway: Look out for extreme mood changes and sudden actions as signs of BPD.
BPD Diagnosis Criteria
Diagnosing BPD requires meeting specific criteria outlined in the DSM-5, a guide healthcare professionals use. A diagnosis is considered when there’s a pattern of instability in relationships, self-image, and affect, along with marked impulsivity. At least five of the following symptoms must be persistent:
- Fear of abandonment
- Unstable relationships
- Disturbed sense of self
- Impulsive behaviors
- Recurrent suicidal behavior or self-harm
- Affective instability
- Chronic feelings of emptiness
- Inappropriate, intense anger
- Transient, stress-related paranoia or severe dissociative symptoms
Key Takeaway: Diagnosis entails a consistent pattern of instability across various aspects of life.
The Role of Mirroring in BPD
Mirroring unconsciously imitates another’s behavior, such as gestures, speech patterns, and emotional expressions. For those with BPD, mirroring can stem from a desire for affiliation or empathy. It may also serve as a strategy to avoid abandonment or to forge a connection, often due to an unstable self-image.
- Key Takeaway: Mirroring can be an emotional response seeking connection or acceptance.
Interpersonal Relationships and BPD
Maintaining relationships can be challenging for individuals with BPD due to their intense fear of abandonment and fluctuating emotions. They might swing between idealizing someone and devaluing them, making relationships turbulent. Empathy and clear communication are vital for managing these dynamics.
- Key Takeaway: Patience and understanding go a long way in relationships affected by BPD.
The Concept of Self in BPD
A stable sense of self is often elusive in BPD, leading to an unstable self-image. Self-awareness can fluctuate, impacting self-reflection and authenticity. Without a coherent understanding of identity, individuals may constantly shift their attitudes and beliefs to match those around them.
- Key Takeaway: An ever-changing view of oneself is standard and can add to the relational strain.
Attachment Styles in BPD
Different attachment styles can be observed in BPD, often leaning towards insecure or disorganized types. This stems from early relationship dynamics with caregivers and can affect adult relationships, perpetuating the cycle of instability and fear of abandonment.
- Key Takeaway: Recognizing one’s attachment style can unlock strategies for more stable relationships.
 BPD and Emotional Regulation
BPD and Emotional Regulation
Emotional regulation is a significant challenge in BPD. Feelings can escalate quickly, and without effective coping mechanisms, individuals may react in ways they later regret. Strategies such as mindfulness, therapy, and emotional regulation skills can provide relief and greater control.
- Key Takeaway: Learning to regulate emotions is possible and crucial for managing BPD.
Narcissistic Mirroring vs. BPD Mirroring
While both narcissistic and BPD mirroring involve imitating others, their motivations differ. Narcissistic mirroring often aims at manipulation or self-aggrandizement. In contrast, BPD mirroring usually seeks connection or fears rejection, rooted in an unstable self-image and intense need for acceptance.
- Key Takeaway: Understanding the intent behind mirroring can clarify misunderstandings in relationships.
Treatment and Management
Managing Borderline Personality Disorder (BPD) requires a comprehensive approach that combines different treatments and strategies aimed at improving emotional regulation, establishing a more stable sense of self, and enhancing interpersonal relationships. You’ll find that the right combination of therapies and support can significantly help control the symptoms and improve the quality of your life.
 Psychotherapy Approaches
Psychotherapy Approaches
Various psychotherapy methods have proven effective in treating BPD, and two prominent ones are:
- Dialectical Behavior Therapy (DBT): DBT is a type of cognitive-behavioral therapy tailored explicitly to BPD. It focuses on teaching skills to cope with stress, control emotions, and improve relationships.
- Key Takeaway: DBT helps build emotional regulation and impulsivity control toolset.
- Cognitive Behavioral Therapy (CBT): CBT assists in identifying and changing harmful thought patterns, leading to better emotional control and reduced problematic behaviors.
- Key Takeaway: Through CBT, you can reshape your thinking and behavior patterns to improve your emotional health.
Medication and BPD
Medication isn’t the primary treatment for BPD, but it might be used to address specific symptoms or co-occurring conditions:
- Antidepressants: Antidepressants can help balance mood swings and reduce feelings of depression or anger.
- Key Takeaway: Although not a cure for BPD, medications can provide symptom relief.
Developing Coping Strategies
Establishing healthy coping mechanisms is vital for managing BPD symptoms:
- Identify triggers that destabilize your emotions.
- Use mindfulness to stay present and reduce impulsive reactions.
- Engage in physical activity to help regulate stress and improve mood.
- Key Takeaway: Coping strategies empower you to deal with difficult emotions and foster a sense of control.
 The Importance of Professional Help
The Importance of Professional Help
Seeking professional help isn’t a sign of weakness but a step toward healing:
- Therapists can offer guidance on therapeutic interventions suitable for your needs.
- Group therapy provides a sense of belonging and an opportunity to practice interpersonal skills in a safe environment.
- Key Takeaway: Professional help is a cornerstone of effective BPD treatment, offering expertise and a supportive network.
Lifestyle Modifications and Support
Your lifestyle choices and support systems play an indispensable role in BPD management:
- Build a steady sleep, meal, and exercise routine to foster stability.
- Cultivate a support network of friends, family, or support groups who understand your challenges.
- Key Takeaway: A stable routine and supportive relationships contribute immensely to your ability to manage BPD.
Social Dynamics and BPD
Borderline Personality Disorder (BPD) profoundly affects your social interactions and the way you form relationships. Your intense emotions can draw people to you and push them away, impacting your social life and sense of identity.
Impact of BPD on Social Interactions
When you have BPD, you might find that your interactions with others are like riding an emotional rollercoaster. Your fear of abandonment and emotional response can lead to intense, unstable relationships. Here’s what you may notice:
- Intense emotional attachments: You might form quick and intense attachments to others, only to find these feelings change unexpectedly.
- Fear-driven responses: A deep fear of abandonment can cause you to misinterpret neutral or even positive social cues as signs of neglect or rejection.
Key Takeaway: Your fear of abandonment can significantly impact the stability of your social interactions, but recognizing these patterns can be the first step toward more balanced relationships.
 BPD and the Quest for Belonging
BPD and the Quest for Belonging
The desire for belonging and affiliation is particularly acute if you’re living with BPD. Here’s how this need can manifest:
- Seeking acceptance: You may go to great lengths to feel accepted and avoid social rejection, which could sometimes lead to disregarding your needs or values.
- The chameleon effect: This might sometimes result in ‘mirroring’ others, adapting your interests, opinions, and even your behavior to fit in and feel part of a group.
Key Takeaway: You strive for inclusion and fear being alone, yet knowing who you are apart from the group is crucial for your well-being.
Understanding and Responding to Rejection
Handling social rejection is often more challenging when you’re managing BPD. Your emotional response to rejection can be intense:
- Heightened sensitivity: You may interpret a friend’s busy schedule or a missed call as personal neglect.
- Theory of Mind: It may be harder to understand that others’ intentions may not match your assumptions about their non-verbal behavior.
Key Takeaway: Understanding that not every slight is intentional can help reduce the pain of perceived social rejection.
Mirroring and Identity Formation
If you’re coping with BPD, you might find that ‘mirroring,’ or reflecting the behavior and emotions of those around you, plays a significant role in how you forge your identity:
- Searching for a stable self: Without a sound sense of self, you might rely on others’ behaviors and characteristics to define your own, often referred to as the ‘chameleon effect.’
- Entrepreneurs of identity: In a way, you become an entrepreneur of identity, constantly adjusting your persona to fit different social contexts.
Key Takeaway: While mirroring can help you blend in and find common ground, it’s also essential to discover and cultivate your sense of identity.
Research and Perspectives
In this pivotal section, you’ll discover how current research decodes BPD’s roots, the latest therapeutic breakthroughs, and how BPD intersects with other mental conditions.
Exploring the Etiology of BPD
Researchers are keenly investigating the causative factors behind Borderline Personality Disorder (BPD). This helps to understand the intricacies of the disorder and, in turn, supports more effective interventions. Data points to both genetic and environmental factors, like childhood neglect, playing pivotal roles in the development of BPD. For instance:
- Genetics: Twin studies suggest a heritable component to BPD.
- Environment: High rates of early trauma and neglect among individuals with BPD are reported.
Key takeaway: Acknowledging the intertwined genetic and environmental factors offers a clearer picture of why BPD arises.
Innovations in BPD Treatment
In the sphere of treatment, strides in psychotherapy emerge as a beacon of hope for those grappling with BPD. Two notable approaches include:
- Dialectical Behavior Therapy (DBT): A modality that blends cognitive-behavioral strategies with mindfulness and ensures skills for managing emotions are learned.
- Schema Therapy: Targets maladaptive belief systems possibly arising from childhood experiences.
Medications may be prescribed primarily for managing specific symptoms rather than the disorder itself.
Key takeaway: Personalized psychotherapy remains the cornerstone of BPD treatment, with medication serving as a supportive tool.
The Relationship Between BPD and Other Disorders
Understanding BPD’s relationship with other disorders is critical for accurate diagnosis and intervention. Research highlights overlap with conditions like:
- Mood Disorders: BPD patients frequently experience intense mood swings.
- Schizophrenia Spectrum Disorders: Some symptoms, like paranoia, can appear in both BPD and schizophrenia spectrum conditions.
Highlighting these overlaps helps healthcare providers distinguish BPD from related personality and mental disorders for better-tailored treatments.
Key takeaway: Discerning the nuances between BPD and other disorders is essential for ensuring proper care and management.
Personal Experiences and Stories
When it comes to Borderline Personality Disorder (BPD), the unique stories of those who live with it can shine a light on the complex nature of this condition. These narratives often underscore the importance of understanding and managing symptoms like emotional dysregulation and impulsivity.
Living with BPD
BPD can make your life feel like you’re on an emotional rollercoaster. The intense mood changes can be hard to predict and even harder to explain to others. Here are a few key points from those who live with BPD:
- Feelings of emptiness: You might feel a chronic sense of emptiness, like an unfillable gap inside you.
- Frequent mood swings: Your emotions can shift rapidly, and these mood swings can be pretty exhausting.
One individual described their struggle with relationships, “The fear of abandonment can make me act in ways I later regret, like sending too many texts or asking for reassurance more often than feels ‘normal.'”
Here’s a key takeaway: If you’re facing similar challenges, know that you’re not alone and that these experiences are part of living with BPD.
Journey to Recovery
Recovery stories often provide hope and highlight the effective coping mechanisms and therapies that can lead to improvement. The pursuit of professional help is a common theme:
- Therapy: Engaging in therapy like Dialectical Behavior Therapy (DBT) can equip you with better emotional regulation tools.
- Support systems: Building a solid network of friends, family, and professionals can provide you with the necessary safety net.
A person shared, “DBT helped me to handle my impulsivity and to think before acting, which greatly improved my relationships.”
Remember this takeaway: Recovery is a personal journey made step by step, with help from professionals and using coping strategies.
Resources and Support
When you’re grappling with Borderline Personality Disorder (BPD) mirroring, knowing where to turn can make a world of difference. It’s about finding support that resonates with your experience and educational tools to help you navigate your symptoms. Let’s explore the avenues that can offer you assistance and connection.
Finding Help and Support
Seeking professional help is a crucial step in managing BPD symptoms. Therapy, especially with therapists specializing in BPD, provides a foundation for understanding and working through the issues associated with mirroring:
- Look for Therapists: Find a professional experienced in Dialectical Behavior Therapy (DBT) or other BPD-specific therapeutic methods.
- Group Therapy: Consider joining a group therapy session where you can share experiences and strategies with others who understand your journey towards feeling a sense of belonging.
Key takeaway: Professional therapy offers you tailored strategies and coping mechanisms to deal with BPD mirroring.
Educational Materials and Advocacy
Educating yourself on BPD can empower you and those around you. Knowledge can foster understanding and advocacy:
- Research: Dive into books, articles, and studies about Borderline Personality Disorder to better comprehend your symptoms.
- Advocacy Groups: Connect with organizations dedicated to BPD to stay informed on the latest research and resources.
Key takeaway: Staying informed through educational materials bolsters your ability to advocate for yourself and connects you with the latest BPD research.
Online and Community Support Networks
In the digital age, finding support can be as simple as connecting online or finding local groups:
- Online Forums: Engage in conversations, ask questions, and build networks on platforms geared towards mental health support.
- Local Support Groups: Look for community meet-ups or support groups where you can find belonging and shared experiences.
Key takeaway: Online and community networks can be a significant source of support, offering you a sense of belonging and connection with others who understand your struggles.
Conclusion
Borderline Personality Disorder (BPD) presents unique challenges, but embracing therapy can lead to significant personal growth. Your journey towards a healthier self often includes:
- Identifying triggers
- Learning coping mechanisms
Therapy as a Tool
You’re not alone on this path. In therapy, you develop strategies for:
- Navigating relationships: Understand how mirroring is an expression of BPD and not your whole identity.
- Self-advocacy: Learn to voice your needs assertively.
Personal Growth
As you progress, you’ll notice:
- A sense of identity solidifying.
- Improved relationship management skills.
Future Directions
Here’s what to look forward to:
- Expanding self-awareness.
- Embracing life’s complexities without losing your sense of self.
Remember, your journey is as unique as you are. Stay open to change and growth.
Key Takeaway: Engage with therapy—it’s a powerful ally in your quest for well-being.
Frequently Asked Questions
When exploring Borderline Personality Disorder (BPD), understanding how individuals interact with others is crucial. Among several behaviors, ‘personality mirroring’ is a significant area of interest due to its complexity and impact on relationships.
What is personality mirroring, and how is it related to BPD?
Personality mirroring occurs when someone with BPD subconsciously imitates the behaviors, mannerisms, or attitudes of those around them. This might stem from an intense desire for acceptance or fear of abandonment, which are common feelings associated with BPD.
- Key takeaway: Mirroring is a coping strategy for individuals with BPD to feel connected to others.
How does someone with BPD typically behave during an episode?
During an episode, a person with BPD may exhibit extreme emotional reactions, impulsive actions, and varying degrees of anger, depression, or anxiety. You might notice rapid mood swings and unpredictable behavior.
- Key takeaway: Episodes can be intense and present a rollercoaster of emotions and actions.
Can people with BPD unintentionally mimic others’ behaviors, and what triggers this?
Yes, individuals with BPD might unintentionally mimic others, driven by deep-rooted fears of rejection or loss of identity. This mirroring can be triggered by stressful situations, intimate settings, or when around people they wish to impress or connect with.
- Key takeaway: Stress and the desire for connection can trigger unintentional mirroring.
Are individuals with BPD more prone to using mirroring as a form of manipulation?
It’s a misconception that mirroring is always manipulative. While some with BPD may mirror with an intent to manipulate, many do it unknowingly as a way to relate to others, not to deceive or exert control.
- Key takeaway: Not all mirroring is manipulative; it’s often an unconscious behavior.
What treatments are available for managing mirroring behaviors associated with BPD?
Treatment options for BPD and associated mirroring behaviors include:
- Dialectical behavior therapy (DBT) helps learn to manage emotions and reduce relationship conflicts.
- Cognitive-behavioral therapy focuses on altering negative thought patterns and behaviors.
- Key takeaway: Therapy aims to understand and change mirroring behaviors for healthier relationships.
Why might a friend with BPD seem to copy my behavior or personality traits?
Your friend may mirror your behavior or traits to strengthen the connection with you or to feel a sense of belonging. It’s essential to approach this behavior compassionately, knowing it likely stems from their fear of being alone or misunderstood.
- Key takeaway: A friend with BPD often mirrors behavior as a way to foster closeness with you.
- Breaking the Silence: Why Men’s Mental Health Matters More Than Ever - April 15, 2025
- How to Transform a Home’s Patio Space into a Relaxing Space - March 23, 2025
- 5 Strategies to Use a Cell Phone to Help Manage Your Stress - March 23, 2025
This site contains affiliate links to products. We will receive a commission for purchases made through these links.

 Understanding BPD
Understanding BPD BPD and Emotional Regulation
BPD and Emotional Regulation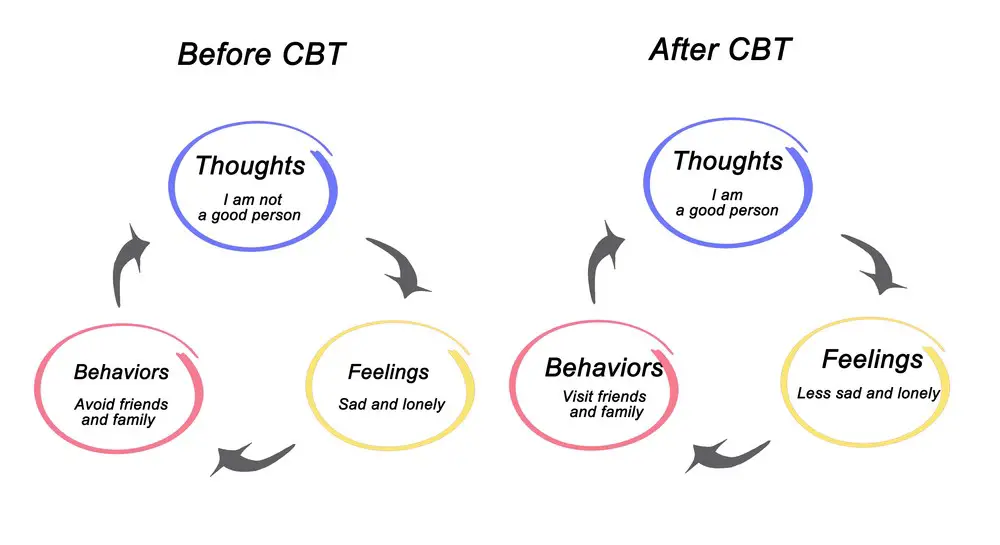 Psychotherapy Approaches
Psychotherapy Approaches The Importance of Professional Help
The Importance of Professional Help BPD and the Quest for Belonging
BPD and the Quest for Belonging
