As a BetterHelp affiliate, we receive compensation from BetterHelp if you purchase products or services through the links provided
Living in a world full of challenges and unexpected situations, it’s no surprise that many people face various trials and tribulations. One such challenge that is particularly common is the experience of a trauma loop. A trauma loop is a brain state that develops a track in your nervous system, often triggered when real-world situations become overwhelming. These loops can form in response to traumatic events, profoundly impacting an individual’s mental health and well-being.
When your body encounters a traumatic event, your limbic system kicks into high gear, leading to a heightened stress response. This creates what is known as a limbic trauma loop. The trauma loop is a mechanism that causes your brain to misidentify threatening stimuli, potentially developing chronic and inexplicable illnesses. The main focus of your brain becomes survival, and other bodily functions may be pushed to the wayside as a result.
Key Takeaways
- Trauma loops are brain states forming tracks in the nervous system triggered by overwhelming situations.
- These loops impact mental health and well-being and can lead to chronic illnesses.
- Limbic trauma loops form when the brain misidentifies threatening stimuli, prioritizing survival over other bodily functions.

Understanding Trauma
Trauma can be a complex and challenging experience, but with a better understanding of how it affects the brain, you can better recognize its impact on your life. This section explores how trauma affects the brain, specifically the limbic system, which consists of the amygdala and hippocampus.
The Brain and Trauma
The limbic system plays a crucial role in processing emotions and memories. When you experience trauma, your limbic system is involved in your body’s stress responses. Two essential parts of the limbic system are the amygdala and the hippocampus:
- Amygdala: This almond-shaped structure is responsible for processing and responding to emotional stimuli, especially fear. When you encounter a traumatic event, your amygdala triggers a fight-or-flight response, releasing stress hormones to help your body prepare for potential danger.
- Hippocampus: Known for its role in memory consolidation, the hippocampus helps store your memories long-term. After a traumatic event, the hippocampus can be impacted by high-stress hormones, potentially leading to memory fragmentation and difficulty recalling specific details of the incident.
In trauma loops, your brain may get stuck in a pattern of continually activating the stress response, even when there’s no current threat. This cycle can be challenging to break, as it causes heightened stress responses and exaggerated reactions to situations that remind you of the initial trauma. Understanding how your brain and trauma interact is key to addressing trauma loops in your life.
Here are a few strategies you can try to help break the cycle of trauma loops:
- Practice mindfulness meditation to help regulate and stabilize your body’s stress responses.
- Engage in deep-breathing exercises to calm the amygdala and reduce overall tension.
- Seek professional support, such as therapy or counseling, to work through your experiences and develop coping mechanisms.
Remember, you’re not alone in experiencing trauma loops; understanding how your brain processes trauma is essential in breaking this cycle.
 Mental Health Consequences
Mental Health Consequences
Complex Trauma
Complex trauma arises from repeated or prolonged exposure to traumatic events, such as child abuse, domestic violence, or wartime experiences. This trauma can significantly affect your mental health, leading to depression, anxiety, and shame. You may struggle with feelings of worthlessness and experience intense nightmares.
To cope with complex trauma, seeking professional help and support from friends or family is crucial. Remember that healing is a process, and you must be patient with yourself. Some strategies to consider include:
- Reaching out to a therapist specializing in trauma
- Engaging in activities that promote relaxation, such as meditation or expressive arts
- Building social connections through support groups or shared hobbies
Post-Traumatic Stress Disorder (PTSD)
Post-traumatic stress disorder (PTSD) is a mental health condition that can develop after experiencing or witnessing a traumatic event. It can cause a range of symptoms, including:
- Intrusive memories or flashbacks of the event
- Avoidance of situations that remind you of the trauma
- Adverse changes in your thoughts and feelings about yourself or others
- Hyperarousal symptoms, such as irritability and difficulty sleeping
If you’re experiencing PTSD, seeking professional help as soon as possible is vital. Early intervention can prevent more severe, long-term mental health issues. Here are some tips for managing PTSD symptoms:
- Consult with a mental health professional trained in evidence-based treatments, such as cognitive processing therapy (CPT) or prolonged exposure (PE) therapy
- Implement strategies to reduce stress and anxiety, such as mindfulness exercises or regular exercise
- Reach out to friends and family members for emotional support
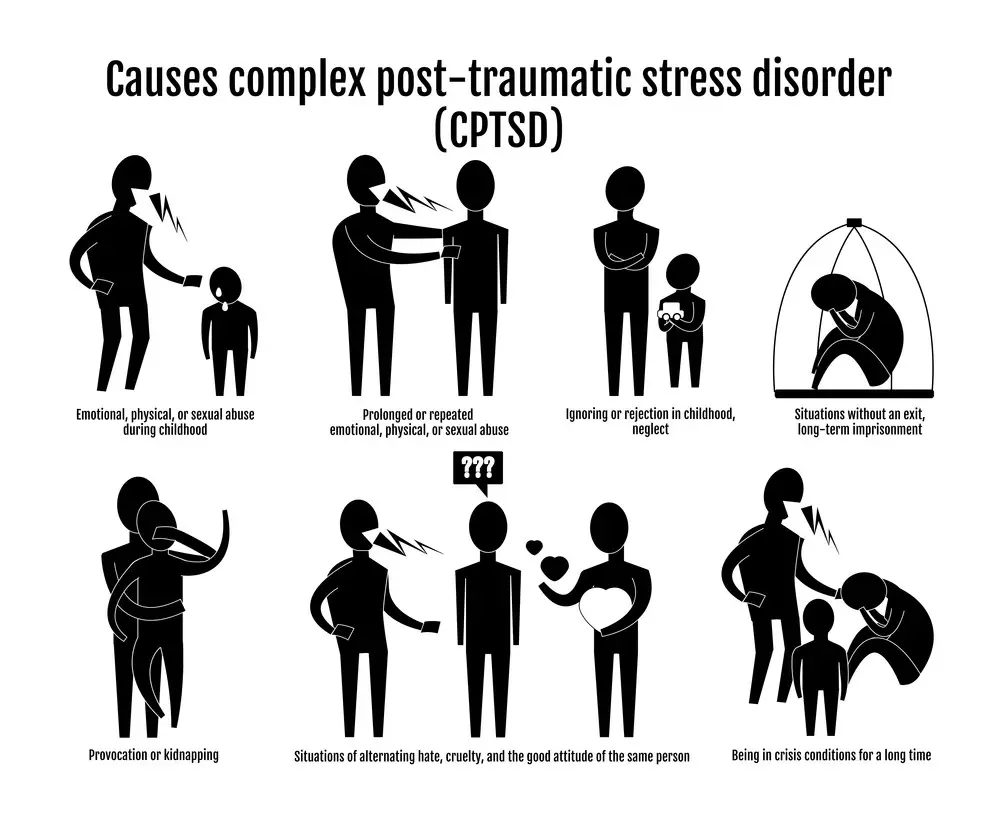
Complex Post-Traumatic Stress Disorder C-PTSD
Complex Post-Traumatic Stress Disorder (C-PTSD), is a variant of PTSD. C-PTSD often develops due to long-term exposure to emotional or physical trauma, like sustained abuse, neglect, or prolonged conflict situations. While it shares many symptoms with PTSD, C-PTSD also features additional elements like:
- Emotional dysregulation: Experiencing significant mood swings or heightened emotional sensitivity
- Negative self-perception: A pervasive feeling of shame, guilt, or worthlessness
- Trouble with relationships: Difficulty forming or maintaining relationships due to mistrust or fear of abandonment
- Loss of faith in systems or people: A generalized feeling of disillusionment or hopelessness
Here are some specific steps you can take to manage C-PTSD:
- Individual Therapy: Seek professionals trained in trauma-focused psychotherapies, such as Dialectical Behavior Therapy (DBT).
- Group Support: Besides individual therapy, support groups offer a sense of community and understanding you might not find elsewhere.
- Healthy Coping Mechanisms: Learn and utilize coping mechanisms that can help you manage emotional dysregulation. Techniques like deep breathing exercises and grounding methods can be invaluable.
- Stay Educated: Knowing more about C-PTSD can empower you to take control of your symptoms. Understanding the science behind what you’re experiencing can make the emotional aspects more manageable.
- Consult Loved Ones: Open communication with trusted friends and family can help your recovery journey. Their emotional support can be a pillar you can lean on.
Whether it’s PTSD or C-PTSD, getting the appropriate help is the first step to regaining control of your life. Both conditions are treatable, and you can move toward a happier, healthier future with the proper support.
The Body’s Response and Coping Mechanisms
When experiencing a trauma loop, your nervous system activates the stress response, alerting your body and shifting into survival mode. This response can manifest in various ways, such as intense fear, anxiety, and dissociation. To better understand this process, let’s explore the body’s response and some coping mechanisms you can use.
Firstly, as the nervous system becomes activated during a traumatic event, you may experience a surge of adrenaline and cortisol, preparing your body for action. Your heart rate increases, your breathing quickens, and your muscles tense up. If the perceived threat persists, your body remains on high alert, which can be exhausting and damaging to your health.
Finding ways to calm your nervous system is essential to counteract this stress response. Here are some strategies you can try:
- Deep breathing: Focusing on slow, deep breaths can help regulate your heartbeat and release tension.
- Mindfulness meditation: Observing your thoughts and emotions without judgment can cultivate greater control and support your nervous system’s return to a balanced state.
- Physical activity: Engaging in activities like walking, jogging, or yoga can calm your nervous system by releasing endorphins and promoting relaxation.
Sometimes, when faced with overwhelming stress, your body might cope by dissociation, a defense mechanism where you detach from reality. Dissociation can come in different forms, such as depersonalization (feeling detached from oneself) or derealization (feeling that the world is unreal). To break free from dissociative tendencies, consider these coping techniques:
- Grounding exercises: Techniques like engaging with your surroundings using all five senses can help you reconnect with the present moment and reduce dissociation.
- Journaling: Writing about your thoughts and feelings can be therapeutic and help you process your experiences.
- Therapy: Working with a trauma-informed mental health professional can be beneficial in addressing the root causes of dissociation and developing personalized coping strategies.
Everyone’s experience is different, and discovering what works best for you may take trial and error. Stay patient with yourself and keep seeking support. Contact friends, family, or mental health professionals to help you navigate this challenging time. And, most importantly, be kind and gentle with yourself as you work through these trying experiences.

The Trauma Loop
The Limbic Trauma Loop
The trauma loop, also known as the limbic trauma loop, is the body’s response to traumatic situations. It stems from your limbic system, the brain’s emotional center that plays a significant role in processing emotions, fear, and memory. When you experience a traumatic event, your body develops a heightened stress response that can lead to exaggerated reactions to triggers.
When caught in a trauma loop, repetitive actions and emotions can occur due to unresolved and overwhelming experiences. These loops can cause your anxiety, post-traumatic stress disorder (PTSD), or depression to worsen as your brain continuously misidentifies threatening stimuli.
To better understand the trauma loop, here are some factors that influence these reactions:
- Triggers: Your environment or experiences can trigger traumatic memories, causing you to spiral into heightened sensitivity.
- Fear: Fear plays a significant role in trauma loops, as it feeds into your body’s fight or flight response. This can lead to increased anxiety and a constant state of alertness.
- Emotions: The emotional charge behind your traumatic experiences can contribute to the intensity of the trauma loop, ultimately making it difficult to break the cycle.
To cope with a trauma loop, consider adopting some of the following strategies:
- Recognize your triggers: Develop self-awareness to identify and avoid situations that may trigger your trauma loop.
- Seek professional help: Consult a mental health professional to work through your trauma and develop coping mechanisms.
- Practice self-care: Take care of your physical, mental, and emotional well-being through exercise, meditation, and hobbies that bring you joy.
Remember, it’s essential to understand that you’re not alone in your struggle with trauma loops. Millions of people face similar challenges every day. By learning about the limbic trauma loop and implementing strategies to break free from it, you can take steps to improve your life and overcome the obstacles caused by trauma.
Interventions and Treatment
Medication and Therapy
When dealing with a trauma loop, it’s essential to consider different intervention methods, like medication and therapy, to help break the cycle. Cognitive Behavioral Therapy (CBT) is one of the most effective treatments for trauma-related issues. This therapy focuses on identifying and changing your thought patterns related to traumatic experiences. You’ll work with a therapist to learn new coping strategies and build resilience.
Another therapy option is Eye Movement Desensitization and Reprocessing (EMDR). This approach involves processing traumatic memories while focusing on specific eye movements, which helps rewire your brain’s response to the trauma.
If you’re struggling with severe symptoms, like anxiety or depression, medications might be a helpful addition to therapy. Some common medications for trauma-related issues include antidepressants, anti-anxiety medications, and sleep aids. Remember, always consult with your healthcare provider before starting any medication.
Key takeaway: Explore different therapy options, like CBT and EMDR, and consider discussing medication with your healthcare provider if needed.
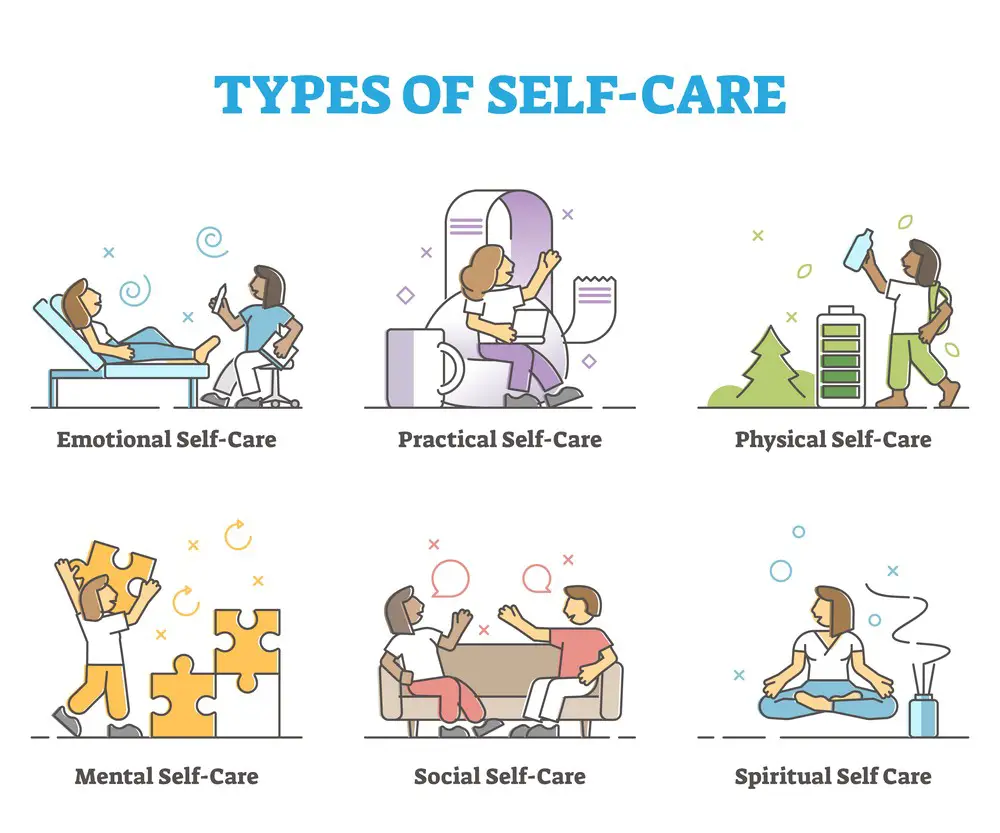
Self-Care Practices
In addition to professional interventions, incorporating self-care into your daily routine can be crucial in managing trauma symptoms and breaking the loop. Here are some tips to promote self-care:
- Meditation: Meditation can help reduce stress, increase self-awareness, and improve emotional health. You can start with a few minutes daily and gradually increase your practice.
- Physical activity: Regular physical activity, like walking, swimming, or yoga, can help reduce anxiety and depression by releasing feel-good endorphins.
- Connection: Connecting with supportive friends, family, or support groups can provide the emotional comfort and understanding necessary for healing.
- Journaling: Writing about your feelings, thoughts, and experiences can help you process trauma and better understand your emotions.
Developing a self-care plan tailored to your needs and preferences might take some time, but it’s worth the investment. Be patient, and try different strategies to find what works best for you.
Key takeaway: Integrate self-care practices, like meditation, physical activity, connecting with others, and journaling, into your daily routine to support your healing process.
The Importance of Support
Trauma can create a vicious circle, and getting out of it requires support and understanding. Building safe and supportive relationships is essential as you heal from traumatic events. Surrounding yourself with people who can provide emotional safety helps break the trauma loop.
Building Safe Relationships
A crucial step in overcoming trauma is creating a safe space with relationships that provide the necessary support. Here are a few tips on building and maintaining safe relationships in your healing journey:
- Choose wisely: Pick the people who are understanding, compassionate, and nonjudgmental. Look for friends, family members, or professionals who make you feel comfortable and help you discuss your feelings without fear.
- Communicate openly: Be honest about your emotions and experiences with those you trust. Open communication fosters a sense of safety and helps in building solid relationships.
- Set boundaries: Establish healthy boundaries with those around you to ensure that you feel respected and protected. This can include emotional or physical boundaries, depending on your needs.
- Join support groups: Connecting with others through similar experiences can be immensely helpful. Joining support groups creates a sense of community where everybody understands the challenges of overcoming trauma and offers empathy and assistance.
- Remember self-care: Besides fostering safe relationships with others, taking care of yourself is essential. Prioritize your mental and physical well-being by setting aside time for self-care activities and seeking professional help.
By building and nourishing safe relationships, you can create a strong foundation of support that will help you escape the trauma loop. It’s important to remember that the healing process takes time. Surrounding yourself with loving and understanding people can aid in overcoming emotional hurdles and moving towards a better mental health state.
Trauma Recovery
Trauma recovery is a process that can take time and effort, but with the right approach, it’s entirely possible to overcome the effects of traumatic experiences. This section will focus on loop closure and its crucial role in your healing journey.
Loop Closure
Loop closure refers to making sense of and resolving traumatic memories, allowing your mind to move forward without being trapped in a repetitive cycle of distress. It’s an essential aspect of recovery that enables us to regain some control over our lives and improve our mental well-being. Here’s how you can work towards loop closure:
- Identify the trauma loop: Pay attention to your thoughts, emotions, and behaviors that keep taking you back to the traumatic event. It could be specific triggers or constant rumination about the incident.
- Seek professional help: Working with a therapist or counselor experienced in trauma recovery is crucial. They can help guide you through the process, providing new insights, coping strategies, and support.
- Implement grounding techniques: When you notice yourself slipping into a trauma loop, use grounding techniques to bring yourself back to the present. Examples include deep breathing exercises, focusing on the sensations in your hands and feet, or repeating an affirming mantra.
- Challenge negative thoughts: As you become more aware of your trauma loops, notice the thoughts that keep you stuck. Work on challenging these negative thoughts and replacing them with more balanced perspectives.
- Find healthy outlets: Engaging in activities that help you process your emotions and build resilience can be highly beneficial. Consider journaling, joining a support group, or practicing mindfulness exercises.
- Be patient: Trauma recovery is not a linear process; it takes time to achieve loop closure. Remember that setbacks are a normal part of the journey, and you must be gentle with yourself as you navigate this challenging time.
In summary, loop closure is an essential aspect of trauma recovery that can help improve the overall quality of life. Being proactive, working with a professional, and practicing self-care strategies will ultimately enable you to move forward and heal from the past. Stay encouraged, and remember that every step you take is a step closer to breaking free from the trauma loop.
In The Context of Trauma Centers
When it comes to trauma loops, understanding how they relate to trauma centers is crucial. Trauma centers play a vital role in addressing the needs of patients experiencing trauma loops. Let’s explore how trauma centers incorporate trauma program evaluation in their approach to care.
Trauma Program Evaluation
A vital aspect of a trauma center’s operations is its trauma program, which involves performance improvement practices. Performance improvement helps ensure that the treatment process for trauma loops is efficient and effective. To provide the best care, trauma centers continuously evaluate and adjust their trauma programs based on data and feedback. Here are some aspects to consider in a trauma program evaluation:
- Identifying areas for growth: It’s essential to assess current practices and identify potential areas where improvements could be made. This could involve analyzing patient outcomes, considering staff feedback, or reviewing the resources available at the center.
- Setting measurable goals: Once areas for improvement have been identified, set specific, measurable goals to help drive the performance improvement process.
- Monitoring progress: Regularly review data and feedback to ensure that the trauma center’s improvement efforts are moving in the right direction. Make any necessary adjustments to ensure that goals are being met.
By constantly evaluating the trauma program and striving for improvement, a trauma center can provide better care to patients experiencing trauma loops. As a patient or a caregiver, you can feel more confident knowing that these centers are committed to continuous excellence in their approach to trauma care.
Underlying Challenges
Childhood and Sexual Abuse
When you face complex trauma, especially childhood or sexual abuse, it’s essential to recognize the underlying challenges. These include the potential for your brain and nervous system to become stuck in a trauma loop, making healing particularly difficult.
In cases of childhood abuse, the brain develops in an environment of fear, pain, and instability, making it difficult to establish a sense of safety and trust in later life. This affects your emotional and mental health and your ability to form healthy relationships with others.
When it comes to sexual abuse, the experience often leads to a distorted view of self-worth and personal boundaries, further complicating the healing process. Both childhood and sexual abuse contribute to the development of complex trauma, a condition that poses unique challenges and requires specialized care.
Here are some key points to consider:
- The brain becomes rewired following trauma, making healing more challenging.
- Emotional and mental health may be impacted, affecting relationships and trust.
- A distorted sense of self-worth and personal boundaries can result from sexual abuse.
Takeaway: Addressing the underlying challenges of complex trauma, especially when it involves childhood or sexual abuse, is crucial for recovery. Understanding these challenges allows for a holistic approach to healing that targets the deep-rooted effects of trauma on the brain, emotions, and relationships.
Advanced Diagnostic Tools
As you explore the world of trauma diagnosis and treatment, you’re bound to encounter a variety of advanced diagnostic tools that can help you navigate this complex field. One primary tool that’s of significant importance is the CT scan.
A CT scan, or computed tomography scan, is a non-invasive imaging technique that provides detailed cross-sectional images of areas in your body. This tool is especially useful in assessing traumatic injuries, as it can visualize internal organs, blood vessels, bones, and soft tissues.
When dealing with trauma patients, a prompt and accurate diagnosis is crucial. With today’s technology, there are several state-of-the-art diagnostic tools available to help you achieve this:
- CT scans: As mentioned, CT scans are instrumental in diagnosing various traumatic injuries. They can detect fractures, internal bleeding, organ damage, and other life-threatening conditions.
- Ultrasonography: This imaging technique, which uses high-frequency sound waves to visualize internal structures, is particularly helpful in diagnosing blunt abdominal trauma. In emergency departments, a focused assessment with sonography for trauma (FAST) exam is often used to assess patients with suspected injuries quickly.
- Trauma screening instruments: To better understand a patient’s history of trauma exposure and its effects, experts like Dr. Joseph Spinazzola have developed and validated various instruments. These tools can assist therapists, researchers, and students in their work.
- Emergency ultrasound: In instances of abdominal and thoracic trauma, emergency ultrasound can be a valuable diagnostic tool. It’s non-invasive and allows for quick visualization of any internal injuries.
Remember, utilizing these advanced diagnostic tools can enhance the accuracy and efficiency of your trauma diagnosis process, ultimately improving patient outcomes. So, it’s vital to stay updated with the latest advancements and ensure you’re providing the best possible care.

When to Wave the White Flag: Signs You Might Need Therapy
Sometimes, recognizing that you need professional help isn’t as obvious as a neon sign. But subtle clues can whisper—or shout—that it’s time to chat with a therapist.
- You’re Stuck in the Mud: You know that feeling of walking through a foggy swamp in your mind? You’re making little to no progress, and it’s frustrating.
- The Emotional Rollercoaster: One minute, you’re elated; the next, you’re in tears. Take note if your emotions are more unpredictable than a game of roulette.
- Hide and Seek with Happiness: If joy feels like a stranger you’re struggling to invite over, that’s a glaring red flag.
- Friends as Sounding Boards: Loved ones are great for venting, but it’s time for a professional intervention if your conversations become crisis hotlines.

Let’s Make a Deal: Setting Goals for Therapy
Goal-setting isn’t just for business meetings or New Year’s resolutions; it’s also a cornerstone of successful therapy. Let’s break down how to set practical and achievable aims.
- Target the Bullseye: Clearly define what you’re hoping to accomplish. A goal like “feel better” is admirable but vague. Try to sharpen it to something like, “Manage my anxiety triggers in social settings.”
- Small Steps, Big Leaps: Aim for incremental progress. Celebrate the tiny wins; they add up.
- The Flexible Framework: Goals aren’t set in stone; they’re more like clay. Revisit, reshape, and reformulate as needed.
The Progress Puzzle: How to Know You’re Moving Forward
Recognizing progress can be like spotting a chameleon in a jungle—elusive and hard to see unless you know what to look for.
- The Aha Moment: There’s this sudden clarity, a moment when you say, “Hey, I dealt with that situation much better this time!”
- Check the Rearview Mirror: Compare your current mental and emotional state to where you were when you started. The distance between the two can be astonishing.
- The Lighter Load: The burdens you’ve been carrying start to feel a bit lighter. It’s like emotional weight loss.
- Validation Station: When people close to you notice the changes—even without knowing you’re in therapy—that’s a pretty strong indicator that your work is paying off.
So, whether you’re just contemplating therapy or already sitting on that proverbial couch, these guidelines can help you navigate the journey. Remember, the road to better mental health is a marathon, not a sprint. Take your time, and don’t forget to celebrate the milestones.
Frequently Asked Questions

How do I complete the Trauma Loop walkthrough?
To complete the Trauma Loop walkthrough, you’ll want to start by understanding the concept of trauma loops and their impact on your emotional well-being. To do this, you could research articles and books by mental health professionals or talk to a therapist. Once you have a solid foundation, you can use different strategies to cope with and break free from trauma loops, such as grounding techniques, mindfulness practices, and seeking support from a mental health professional or a support group. Remember, overcoming trauma loops is a process that might take some time, so be patient.
What is the Trauma Loop Limit Chancellor?
The term “Trauma Loop Limit Chancellor” seems to combine unrelated words or a fictional concept. If you’re seeking information on trauma loops, you may want to explore the causes, symptoms, and treatment options mentioned in this article.
How do I achieve an S rank in Trauma Loop?
The term “S rank in Trauma Loop” is unclear. If you are referring to achieving a high level of success in managing trauma loops, then focus on building self-awareness, practicing self-care, and seeking help from mental health professionals to create a personalized plan. Everyone’s journey to healing is different, so it’s essential to find the techniques and solutions that work best for you.
What is the Trauma Loop Ambassador in Cruelty Squad?
“Trauma Loop Ambassador in Cruelty Squad” seems to be a fictional character, concept, or term not directly related to trauma loops and mental health. For help with trauma loops, please refer to the information on understanding and dealing with these emotional patterns.
What are the different Cruelty Squad endings?
Cruelty Squad appears to be a video game unrelated to trauma loops and mental health. Separating fictional scenarios from real-life experiences is essential when discussing emotional well-being. Consider searching for information related explicitly to Cruelty Squad if you want to explore its storylines and endings.
How do I get Cruelty Squad ending 3?
To find information on achieving a specific ending in the Cruelty Squad game, you may want to explore gaming forums, walkthroughs, and guides dedicated to that topic. Remember, this article focuses on understanding, managing, and healing from trauma loops in real-life situations.
Jacob Maslow
After surviving the traumatizing events of 9/11, I took it upon myself to heal through helping others. I’m the primary caregiver of my children and understand from first-hand experience the lonely paths you have to walk as a partner and parent when leaving an unhealthy relationship.
We’re all echoing in a dark space that doesn’t have to be this empty, and that’s been my mission since finding solace and recovery in therapy: To help comfort others who are still in shock and at the prime of their struggle.
I came across BetterHelp after searching for this type of community. I wanted to belong to a body of proactive therapists and supportive therapy veterans that allowed me to see other sides of the story.
It was unconventional, and that’s what attracted me most. During my most challenging times, when my ex-wife completely cut me off from my children, I found comfort and clarity through BetterHelp.
Instead of being chained to a strict therapist recommendation, I was in charge of who I felt understood my struggle most. That allowed me to find my true peace, as I was reunited with those who read behind my words and had first-hand experience with my trauma.
Recovery is a choice; with BetterHelp, that choice will be a few clicks away. You can join their couples-oriented platform, Regain.us, for those stuck with family estrangement and toxic relationship patterns.
- Breaking the Silence: Why Men’s Mental Health Matters More Than Ever - April 15, 2025
- How to Transform a Home’s Patio Space into a Relaxing Space - March 23, 2025
- 5 Strategies to Use a Cell Phone to Help Manage Your Stress - March 23, 2025
This site contains affiliate links to products. We will receive a commission for purchases made through these links.


 Mental Health Consequences
Mental Health Consequences