Obsessive-compulsive disorder (OCD) is a challenging mental health condition that affects millions of people worldwide. Characterized by intrusive thoughts and repetitive behaviors, OCD can have a significant impact on an individual’s quality of life. Many treatment options have been explored, with varying degrees of success, leading researchers to seek alternative approaches to manage this condition.
Ketamine, a drug initially developed as an anesthetic and pain reliever, has attracted attention in recent years for its potential use in treating a variety of mental health disorders, including depression and post-traumatic stress disorder. Now, studies are exploring the possible benefits of ketamine for individuals with OCD. While still in the investigational stage, some early results suggest that ketamine may provide rapid relief from OCD symptoms, opening up new horizons for treatment possibilities.
Key Takeaways
- Ketamine is being explored as a potential treatment for OCD, with some promising early results.
- Studies have shown a fast onset of action and good tolerability of ketamine in treating OCD symptoms.
- More research is needed to fully understand the potential role of ketamine and its long-term effectiveness in managing OCD.
 Understanding Obsessive-Compulsive Disorder
Understanding Obsessive-Compulsive Disorder
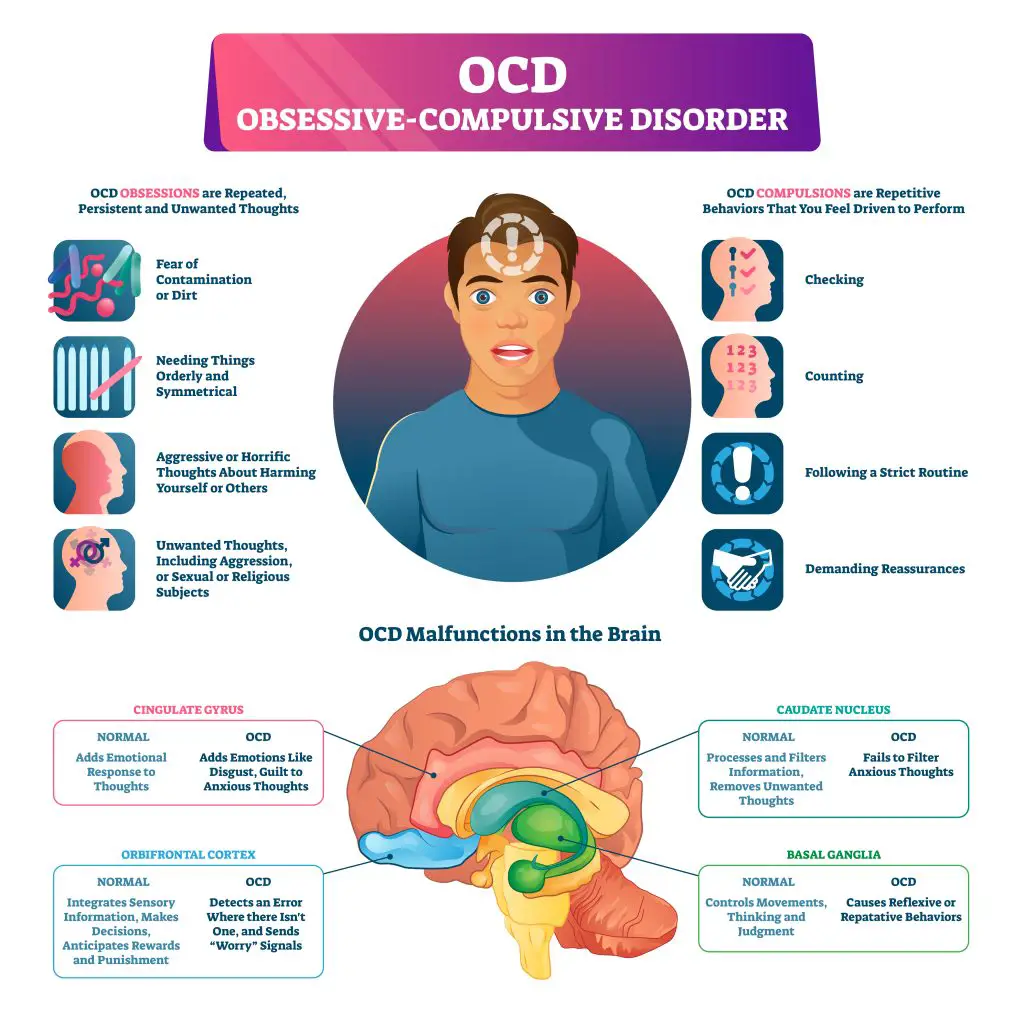
Obsessive-compulsive disorder (OCD) is a mental health disorder that affects people of all ages. It is characterized by two main components: obsessions and compulsions.
Obsessions are recurrent, unwanted thoughts or images that cause anxiety and distress. Common obsessions in OCD include:
- Fear of contamination or germs
- Worries about harm coming to oneself or others
- Unwanted/taboo thoughts about sex, religion, or violence
- Need for symmetry, order, or perfection
Compulsions are repetitive behaviors or mental acts the person feels compelled to perform in response to their obsessions. These actions are aimed at reducing the anxiety caused by the obsessions, but they can sometimes lead to more distress in the long run. Some common compulsions include:
- Excessive hand washing or cleaning
- Checking locks, electrical appliances, or other safety measures
- Repeating words or numbers or counting in a specific pattern
- Rearranging items in a particular order
While everyone has occasional unwanted thoughts or participates in repetitive behaviors, it is the intensity, frequency, and interference caused by these thoughts and behaviors that distinguishes OCD from ordinary experiences. To be diagnosed with OCD, the obsessions or compulsions must cause significant distress or interfere with daily functioning for a substantial amount of time.
OCD is a complex disorder, and understanding its behavioral sciences is crucial for effective treatment. Depending on the severity and individual factors, treatment for OCD may involve therapy, medication, or a combination of both. While some people may find significant relief from their symptoms, others may continue to struggle with obsessions and compulsions throughout their lives. Moving forward, it is essential to recognize the challenges faced by those with OCD, as well as the potential treatments and coping strategies available to them.
 Ketamine: An Overview
Ketamine: An Overview
Ketamine is an anesthetic that has been used for years to induce and maintain anesthesia. Recently, it has gained attention for its potential use in treating mental health conditions, such as obsessive-compulsive disorder (OCD). Ketamine can have hallucinogenic and dissociative effects on some individuals. It’s essential to be cautious when using ketamine, as it also has addictive properties. The substance is racemic ketamine, a mixture of two enantiomers: S-ketamine and R-ketamine. S-ketamine has shown a stronger affinity to receptors and is being further investigated for its therapeutic potential.
When using ketamine, its dissociative effects can lead to a feeling of detachment from one’s body and reality. This may initially be disorienting; however, it can also provide relief from the obsessive thoughts and compulsions that are characteristic of OCD. Ketamine’s mechanisms of action involve the N-methyl-D-aspartate (NMDA) receptors, which modify brain activity. By altering the brain’s neuroplasticity, ketamine has shown promising results in reducing OCD symptoms.
It’s important to note that while ketamine can be effective for some people, it may not be the best option for everyone. Some individuals may experience undesirable side effects, such as hallucinations and heightened anxiety, due to ketamine’s psychoactive properties. Also, because ketamine has addictive potential, it’s crucial to monitor its use in a clinical setting carefully.
When considering ketamine for OCD treatment, healthcare professionals may choose between racemic ketamine and S-ketamine. S-ketamine, the more potent of the two enantiomers, appears to have more significant therapeutic potential due to its increased affinity for NMDA receptors. This has led to further research and investigation into using esketamine, a form of S-ketamine, as a possible treatment for OCD and other mental health disorders.
In summary, ketamine shows promise for treating OCD and other mental health conditions, but it is crucial to use it responsibly and cautiously. Understanding the potential side effects, as well as the dissociative and hallucinogenic aspects of ketamine, can help you and your healthcare provider determine if it’s the right course of treatment for your OCD. Always consult a medical professional when considering new treatment options.
 Ketamine and OCD: The Connection
Ketamine and OCD: The Connection
You might be intrigued to know that ketamine has been making waves in the mental health realm for its potential use in treating obsessive-compulsive disorder (OCD). This relatively newfound connection brings the science of neurobiology and glutamatergic neurotransmission into the spotlight.
The key to this connection lies in ketamine’s effect on NMDA receptors, crucial components in the glutamate system. As someone interested in mental health, you’re likely aware that glutamate is the primary excitatory neurotransmitter in your brain. Ketamine can significantly disrupt the regular glutamate transmission, leading to temporary relief of OCD symptoms.
This relief comes from neuroplasticity, the brain’s ability to change and adapt over time. Ketamine essentially “resets” the neural pathways associated with OCD, allowing for a break from the vicious cycle of obsessions and compulsions. It’s particularly promising for those with refractory obsessive-compulsive disorder, an often debilitating form of OCD that is resistant to conventional treatments.
Here’s a quick summary of the connection between ketamine and OCD:
- Ketamine impacts the glutamate system by blocking NMDA receptors
- This disruption in glutamatergic neurotransmission can reduce OCD symptoms
- Neuroplasticity allows the brain to adapt and shift away from obsessive thoughts and behaviors
One thing to keep in mind is that research on ketamine for OCD is still in its early stages, and not all studies have consistent results. However, the potential benefits of ketamine treatment make it a topic worth exploring in the world of mental health. The unique mechanism of action and potential for fast onset can be a breakthrough for those struggling with OCD when traditional treatments have not provided relief. Remember that it’s crucial to stay informed about ongoing research developments and to consult a mental health professional before considering ketamine therapy for OCD.
Clinical Trials and Studies on Ketamine for OCD
In recent years, there have been several clinical trials and studies exploring the potential of ketamine as a treatment for Obsessive-Compulsive Disorder (OCD). One notable clinical trial was conducted in 2012, where participants with treatment-resistant OCD received ketamine infusions. While the trial showed promising results, it’s important to remember that ketamine is an FDA-approved anesthetic but also an illicit party drug with hallucinogenic effects and potential for abuse.
A systematic review of studies on ketamine for OCD has also been conducted. This review revealed that ketamine may have a fast onset of action and good tolerability, but the principal studies were limited to single-session racemic ketamine treatments administered intravenously. Moreover, the results from these studies have been inconsistent.
Some trials have been randomized controlled trials, comparing the effects of ketamine to placebo in treating OCD. For example, there has been a double-blind, randomized controlled crossover trial where participants were either given ketamine or a placebo. The study found that ketamine had a significant impact on reducing OCD symptoms without the presence of an SRI (serotonin reuptake inhibitor). This finding is consistent with a glutamatergic hypothesis of OCD.
Other research focused on ketamine augmentation of exposure-response prevention therapy for patients with OCD. This pilot study explored the effects of ketamine on N-methyl D-aspartate receptors (NMDAR) and gamma-aminobutyric acid receptors (GABAR). Both pathways play a crucial role in contingency learning, belief updating, and extinction learning, which are important aspects of OCD treatment.
To stay up-to-date with ongoing and potential future studies, you can check websites like clinicaltrials.gov to learn about the latest progress in using ketamine for OCD.
In summary, while the existing studies and clinical trials surrounding ketamine as an OCD treatment show promise, it’s crucial to approach this subject with caution, as the results have been inconsistent and the drug has potential for abuse.
 Ketamine Treatment Procedures for OCD
Ketamine Treatment Procedures for OCD
Ketamine has shown promising results in treating obsessive-compulsive disorder (OCD), and its treatment procedures come in two primary forms: intravenous and intranasal administration.
Intravenous Ketamine Treatment
Intravenous (IV) ketamine treatment involves administering ketamine through an IV line directly into your bloodstream. This method offers a fast onset of action, and the dosage can be tailored to your needs. The treatment process consists of:
- Consult with a mental health professional to evaluate your suitability for ketamine treatment and to discuss the potential risks and benefits.
- Receiving IV ketamine infusions in a controlled clinical environment under the supervision of a healthcare professional. The sessions usually last about 40 minutes, and the dosage will vary depending on your response to the treatment.
- Monitoring your progress throughout the treatment course typically involves a series of infusions over several weeks. Adjustments to the dosage and frequency of treatments may be necessary based on your progress and any side effects experienced.
Intranasal Ketamine Treatment
Intranasal ketamine treatment is a less invasive alternative to intravenous administration. This approach involves spraying a ketamine solution into your nostrils, allowing the drug to be absorbed through the nasal passages. While not as direct as IV administration, intranasal ketamine offers some benefits:
- Intranasal ketamine is generally considered more convenient and comfortable, as it doesn’t require the placement of an IV line. This can make the treatment more accessible for those who are needle-averse or have limited access to clinical settings.
- The intranasal method still allows for a relatively fast onset of action, though it may not be as rapid as the intravenous approach.
When seeking ketamine treatment for OCD, it’s essential to consult with a qualified mental health professional who can guide you through the process, help you weigh the benefits and risks, and determine the most suitable administration method for your specific needs. Ultimately, the goal is to help you alleviate your OCD symptoms and improve your overall well-being.
 Potential Risks and Side Effects of Ketamine Treatment
Potential Risks and Side Effects of Ketamine Treatment
When considering ketamine as a treatment for obsessive-compulsive disorder (OCD), it’s important to be aware of the potential risks and side effects associated with its use. While some studies have shown promising results in treating OCD, there are still concerns regarding its safety and long-term effects.
Physical Side Effects
Ketamine can cause various physical side effects, such as:
- Dizziness
- Nausea and vomiting
- Increased blood pressure, heart rate, breathing, and body temperature
At higher doses, these side effects can become more pronounced and problematic.
Mental Side Effects
As a hallucinogenic substance, ketamine can also lead to alterations in your sensory perceptions, including visual or auditory hallucinations. Feeling detached from yourself, your surroundings, or your environment is also possible.
Unreality and Suicidality
In some cases, ketamine may induce sensations of unreality and disconnectedness from the world. For individuals who are predisposed to suicidal ideation or have a history of suicidality, this disconnection could potentially exacerbate these thoughts or feelings. It’s vital to discuss your mental health history with your healthcare provider before considering ketamine treatment for OCD.
Cognitive Impairment and Dependence
Chronic, high-frequency ketamine use has been linked to cognitive impairment and bladder inflammation. If taken regularly, ketamine can also lead to dependence, so monitoring usage and being aware of the potential for addiction is crucial.
Given these potential risks and side effects, it’s essential to speak with your healthcare provider about whether ketamine is a suitable option for your OCD treatment and to be well-informed about potential side effects before starting the treatment.
The Role of Other Treatments in Managing OCD
While ketamine has shown promise in treating OCD, it’s essential to recognize the variety of other treatment options available. These alternatives play a crucial role in managing OCD symptoms and provide a more comprehensive approach to treatment.
Serotonin and Serotonin Reuptake Inhibitors (SSRIs): Serotonin, a neurotransmitter, significantly impacts mood regulation. As a result, using medications such as SSRI antidepressants, which specifically target serotonin levels, can be effective in managing OCD symptoms. Examples of commonly prescribed SSRIs for OCD include fluoxetine, sertraline, and paroxetine. These medications may take several weeks to exhibit noticeable progress, but they can help manage symptoms more consistently than ketamine.
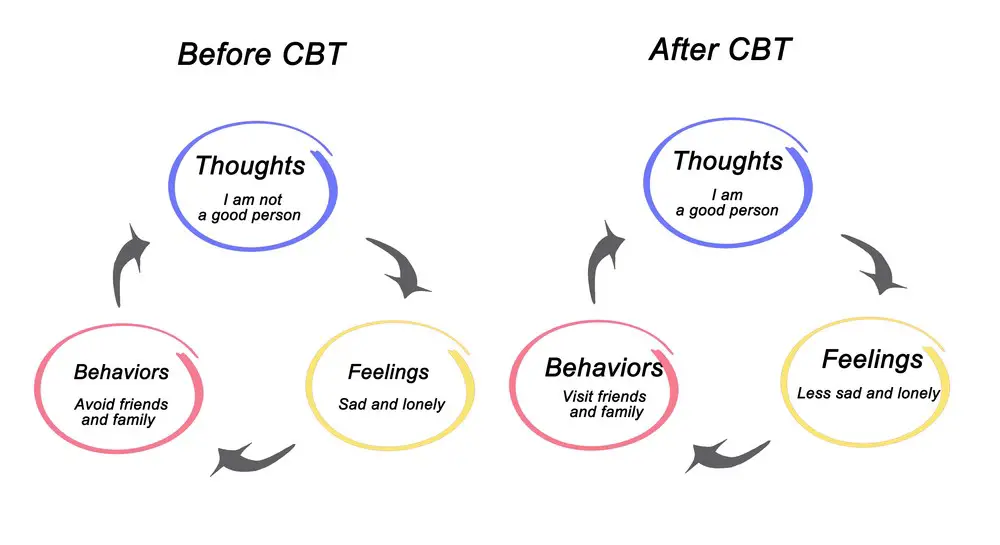 Cognitive Behavioral Therapy (CBT): CBT is a form of psychotherapy that addresses the relationship between thoughts, feelings, and behaviors. It has been proven effective in treating various mental health conditions, including OCD. Through CBT, you will learn to identify and challenge your obsessions and compulsions, ultimately gaining control over your symptoms.
Cognitive Behavioral Therapy (CBT): CBT is a form of psychotherapy that addresses the relationship between thoughts, feelings, and behaviors. It has been proven effective in treating various mental health conditions, including OCD. Through CBT, you will learn to identify and challenge your obsessions and compulsions, ultimately gaining control over your symptoms.
Exposure and Response Prevention (ERP): A specific form of CBT, ERP is a treatment approach where you systematically expose yourself to situations that trigger your obsessions while refraining from performing the compulsive behaviors. Over time, this method helps decrease the severity of your symptoms and can lead to long-lasting improvements.
Other Psychotherapy Approaches: In addition to CBT and ERP, other forms of psychotherapy, such as psychodynamic therapy, can be beneficial for some individuals with OCD. These therapies usually focus on uncovering and addressing the unconscious processes contributing to your symptoms.
Relaxation and Mindfulness Techniques: Learning to manage your stress and anxiety through relaxation techniques, such as deep breathing exercises, progressive muscle relaxation, and guided imagery, can significantly improve your overall well-being. Moreover, mindfulness practices, like meditation and yoga, can help you cultivate a non-judgmental awareness of your thoughts and feelings, reducing the impact of your OCD symptoms.
By incorporating a range of these treatments into your OCD management plan, you can enhance your ability to cope with the challenges of this disorder and achieve an improved quality of life. Consult a mental health professional to determine the most appropriate treatment approach for your needs.

Comorbidity of OCD and Other Psychological Disorders
Obsessive-Compulsive Disorder (OCD) often occurs alongside other psychological disorders, which is called comorbidity. Understanding the comorbidities can help provide better treatment strategies for individuals with multiple disorders. In this section, we will discuss some common comorbidities and their relationship with OCD.
Anxiety and Major Depressive Disorder (MDD): Anxiety and depression are two of the most common disorders that co-occur with OCD. Both anxiety disorders and MDD can have a significant impact on an individual’s daily life, and when combined with OCD, the severity and complexity of symptoms often increase.
PTSD: Post-traumatic stress disorder (PTSD) can also be comorbid with OCD. People who have experienced a traumatic event may develop compulsive behaviors or obsessive thoughts as a way to cope with their distress. This can lead to the development of both PTSD and OCD symptoms in some cases.
Eating Disorders: Eating disorders, such as anorexia nervosa and bulimia nervosa, often co-exist with OCD. These disorders share some common features, like an underlying need for control and obsessive thoughts. The comorbidity of OCD and eating disorders can make the treatment more complex and require an integrated approach.
Mood Disorders and Bipolar Depression: Mood disorders, especially bipolar depression, have been reported to co-occur with OCD in some cases. Individuals with both conditions may experience heightened emotional instability and oscillate between periods of obsessive thoughts, compulsions, and depressive episodes.
Comorbid Depression: Many people with OCD also suffer from comorbid depression. This can make dealing with OCD symptoms more difficult, as the depressive episodes can exacerbate the severity of the obsessive thoughts or compulsive behaviors.
As you can see, the comorbidity of OCD with other psychological disorders is not uncommon, and it’s important to consider these comorbidities when developing treatment plans. Being aware of and addressing these comorbid disorders can help improve the overall mental health of people dealing with OCD.
Future Perspectives in OCD and Ketamine Treatment
As you explore the promising world of ketamine treatment for obsessive-compulsive disorder (OCD), it is essential to investigate future directions in research and clinical practice. To date, reported data has shown a potential for a fast onset of action and good tolerability of ketamine in treating OCD. However, these findings mostly come from single-session racemic ketamine treatments administered intravenously, and the results have been inconsistent.
New treatment approaches are currently being investigated, focusing on ketamine’s therapeutic effect in combination with existing treatments. For example, researchers are exploring how ketamine may enhance extinction-based psychotherapy, such as cognitive-behavioral therapy with exposure and response prevention. By augmenting these therapies, ketamine could lead to more effective outcomes for patients struggling with OCD.
Moreover, the potential use of esketamine, an enantiomer of ketamine, is gaining interest in the treatment of OCD. Recent small studies have reported promising results in treating not only treatment-resistant depression but also OCD and post-traumatic stress disorder. Esketamine’s unique properties may prove beneficial in transforming the landscape of OCD treatments.
When evaluating the effectiveness of ketamine in treating OCD, it’s crucial to consider the measures used to gauge improvement. The Yale-Brown Obsessive-Compulsive Scale (Y-BOCS), a widely accepted assessment tool, is one such instrument used in various studies to measure reductions in symptoms related to OCD. Ensuring the accurate interpretation of these measures will be essential in further research and clinical applications.
In conclusion, keep in mind these critical takeaways as you consider future perspectives in OCD and ketamine treatment:
- Explore the combination of ketamine treatment with existing therapies like extinction-based psychotherapy.
- Investigate the potential of esketamine as an alternative to ketamine for more effective symptom relief.
- Pay attention to assessment tools like the Y-BOCS to evaluate the effectiveness of ketamine and esketamine in treating OCD.
References
One of the primary references for the use of ketamine in OCD treatment comes from Stanford University researcher Carolyn Rodriguez and her colleagues. In 2013, they published their results from the first clinical trial of ketamine for OCD treatment. They discovered that ketamine potentially regulated OCD symptoms as well as depression by affecting the levels of the neurotransmitter glutamate in the brain. They also pointed out the increasing evidence that glutamate plays a significant role in OCD symptoms.
In a PubMed report, a systematic review was conducted to investigate the effects of ketamine in OCD treatment. As a potent N-methyl-D-aspartate (NMDA) receptor antagonist and a glutamate modulator, ketamine offers alternative possibilities for OCD treatment. The review followed the Preferred Reporting Items for Systematic Review and meta-analysis protocols (PRISMA-P) to ensure comprehensive, accurate, and relevant information.
Another study looked at the effects of ketamine in treatment-refractory OCD cases. The open-label trial involved administering a low dose of ketamine (0.5mg/kg IV over 40 minutes) to 10 subjects with treatment-refractory OCD. The response was measured by a significant reduction in OCD symptoms (greater than 35%) and depression symptoms (greater than 50%) from baseline at any time between 1-3 days following the infusion.
Some research has also explored the use of intranasal ketamine in combination with cognitive-behavioral therapy (CBT) for the treatment of refractory OCD. The focus was on agents that modulate glutamate, including the NMDA antagonist ketamine. The study aimed to examine the effectiveness of ketamine as a rapid-acting antidepressant that enhances cellular mechanisms associated with resiliency and the potential for its use alongside CBT.
To summarize, some key references for the use of ketamine in OCD treatment include:
- Stanford University’s Rodriguez and colleagues’ first clinical trial of ketamine for OCD treatment.
- The PubMed report investigated the effects of ketamine in OCD treatment through a systematic review.
- The open-label trial is examining the effects of ketamine in treatment-refractory OCD cases.
- The study on intranasal ketamine and CBT for treatment-resistant OCD.
Frequently Asked Questions
What is the efficacy of ketamine in treating OCD?
Ketamine has shown potential in treating obsessive-compulsive disorder (OCD) symptoms. Some studies have reported a fast onset of action and good tolerability of ketamine for OCD, although the results have been inconsistent. It’s important to note that most research has used single-session racemic ketamine treatments administered intravenously.
Are there clinical trials supporting ketamine use for OCD?
Yes, there have been clinical trials investigating the use of ketamine for OCD. Yale researchers initiated a study that found a substantial, albeit short-term, reduction in OCD symptoms following a single 0.5 mg/kg IV dose of ketamine. However, more research is needed to understand the long-term effects and optimal dosing regimen for using ketamine in treating OCD.
How does ketamine compare to traditional OCD treatments?
Traditional OCD treatments include exposure and response prevention therapy, cognitive-behavioral therapy, and medication like selective serotonin reuptake inhibitors (SSRIs). While ketamine has shown early promise in alleviating OCD symptoms, it should be considered an adjunct or alternative treatment option: the fast-acting and potentially more potent nature of ketamine warrants further study in comparison to traditional OCD treatments.
Is esketamine different from ketamine in treating OCD?
Esketamine is the S(+) enantiomer of ketamine and has a slightly different chemical structure. While both molecules target N-methyl-D-aspartate (NMDA) receptors in the brain, esketamine may have a different binding profile and efficacy. Currently, there is limited research on the use of esketamine for OCD specifically, so it’s challenging to draw definitive conclusions about its effectiveness compared to ketamine.
What are the potential side effects of using ketamine for OCD?
Using ketamine for OCD may lead to several side effects. Chronic and high-frequency ketamine use has been associated with an increased risk of bladder inflammation and cognitive impairment. Taking ketamine regularly can also lead to dependence. It’s essential to understand all potential risks and discuss them with your healthcare professional before starting ketamine therapy.
How is ketamine administered for OCD therapy?
Ketamine for OCD is typically administered intravenously in a controlled medical setting. The standard dose is 0.5 mg/kg, given over a short period. Other methods, such as intranasal or oral administration, may be considered, but efficacy and safety may vary with different routes of administration. Your healthcare provider can recommend the most appropriate method for your situation.
- Is Programming a Stressful Job? - February 21, 2024
- Best Sleeping Positions For Sleep Apnea: How To Improve Your Sleep Quality - February 21, 2024
- Stress vs Anxiety: Understanding the Key Differences - February 19, 2024
This site contains affiliate links to products. We will receive a commission for purchases made through these links.

 Understanding Obsessive-Compulsive Disorder
Understanding Obsessive-Compulsive Disorder Ketamine: An Overview
Ketamine: An Overview Ketamine and OCD: The Connection
Ketamine and OCD: The Connection Ketamine Treatment Procedures for OCD
Ketamine Treatment Procedures for OCD

