As a BetterHelp affiliate, we receive compensation from BetterHelp if you purchase products or services through the links provided
Experiencing a traumatic event can feel like a storm passing through, leaving a trail of emotional upheaval in its wake. Amidst this turmoil, two somewhat shadowy figures often emerge Acute Stress Disorder (ASD) and Post-Traumatic Stress Disorder (PTSD). Though they might seem like distant cousins at first glance, they have distinct features that set them apart. In this blog post, we’re diving into the heart of the matter, exploring the landscape of “Acute Stress Disorder vs PTSD.” Their differences are not just in name but extend to when they appear, how long they stay, and the kind of footprint they leave behind on one’s life.
We aim to untangle the threads of ASD and PTSD, offering a clearer understanding of both, alongside shedding light on effective treatment routes. With a blend of insight and guidance, we hope to offer a helpful companion for those affected on the road towards healing and reclaiming peace of mind.
Understanding Acute Stress Disorder (ASD)
ASD and PTSD are both traumatic disorders but differ in onset, duration, and long-term implications. A thorough grasp of these differences aids in accurate diagnosis and effective treatment.
What Is Acute Stress Disorder?
Acute Stress Disorder (ASD) is a psychological reaction to traumatic events, characterized by manifestations like:
- Flashbacks
- Nightmares
- Detachment, which is one of the dissociative symptoms
- Irritability, often resulting in a negative mood
It takes place within one month of the event and persists for at least three days. Individuals with ASD may experience various symptoms, from intrusive thoughts and flashbacks to emotional numbing and avoidance symptoms associated with the trauma.
Acute Stress Disorder symptoms usually prevail for three days to four weeks, appearing initially within a month after the traumatic incident. To diagnose ASD, specific criteria based on the Diagnostic and Statistical Manual of Mental Disorders (DSM) must be met, including:
- Experiencing a traumatic event
- Displaying at least one symptom of re-experiencing the trauma
- Marked avoidance of trauma-related thoughts or reminders
- Symptoms of anxiety or increased arousal
ASD vs. Normal Stress Responses
Normal stress responses are anticipated reactions to difficult circumstances designed to increase the probability of survival or manage challenging circumstances. The primary distinction between normal stress response and ASD is the duration of symptoms. While normal stress responses are predictable reactions to challenging situations, ASD is characterized by more severe, long-lasting symptoms that hinder daily functioning. The American Psychiatric Association provides guidelines for diagnosing and differentiating these conditions.
ASD is a short-term mental health disorder, transpiring within the first month after a traumatic event, marked by severe, distressing, and dysfunctional responses persisting for under a month. Early attention and treatment for someone with ASD may potentially prevent the eventual development of PTSD. When a professional treatment plan is implemented to treat acute stress disorder, the individual can cultivate skills for managing their disorder before it becomes chronic.
Post-Traumatic Stress Disorder (PTSD)
Posttraumatic stress disorder (PTSD) is a chronic anxiety disorder that develops after exposure to a traumatic event. The following symptoms characterize it:
- Re-experiencing the event
- Avoidance
- Negative thoughts and feelings
- Heightened alertness to danger
Non-PTSD psychopathology is one of the risk factors for subsequent exposure to trauma and developing PTSD. The more prior disorders present, the higher the risk of both exposure and development of PTSD.
Exploring PTSD
Triggered by traumatic incidents, PTSD is typified by enduring PTSD symptoms that can persist for years, impacting an individual’s cognition, emotions, and holistic health. The signs and symptoms associated with PTSD can be categorized into four groups:
- Re-experiencing the event
- Avoidance
- Negative thoughts and feelings
- Heightened alertness to danger, also known as hyperarousal symptoms.
It has been reported that 79.0 percent of women and 88.3 percent of men with a lifetime PTSD diagnosis also had a lifetime diagnosis of one or more Axis I disorders, indicating a high rate of comorbidity between PTSD and other psychiatric disorders.
It is important to note that PTSD can manifest without prior occurrence of ASD.
ASD vs. PTSD: Key Differences
The principal disparities between ASD and PTSD reside in the symptom’s time frame and duration, intensity, and long-standing impacts on an individual’s mental health. Acute Stress Disorder lasts up to one month, whereas Post-Traumatic Stress Disorder can remain for years. Generally, the intensity of symptoms of ASD is less pronounced than that of PTSD, making the difference between PTSD Acute Stress Disorder and less severe acute stress.
Individuals with ASD may be vulnerable to developing PTSD, and those with PTSD may be susceptible to other mental health issues such as depression and anxiety. Early intervention and treatment for ASD may potentially prevent the development of PTSD, while proper management of PTSD can reduce the risk of developing other mental health conditions.
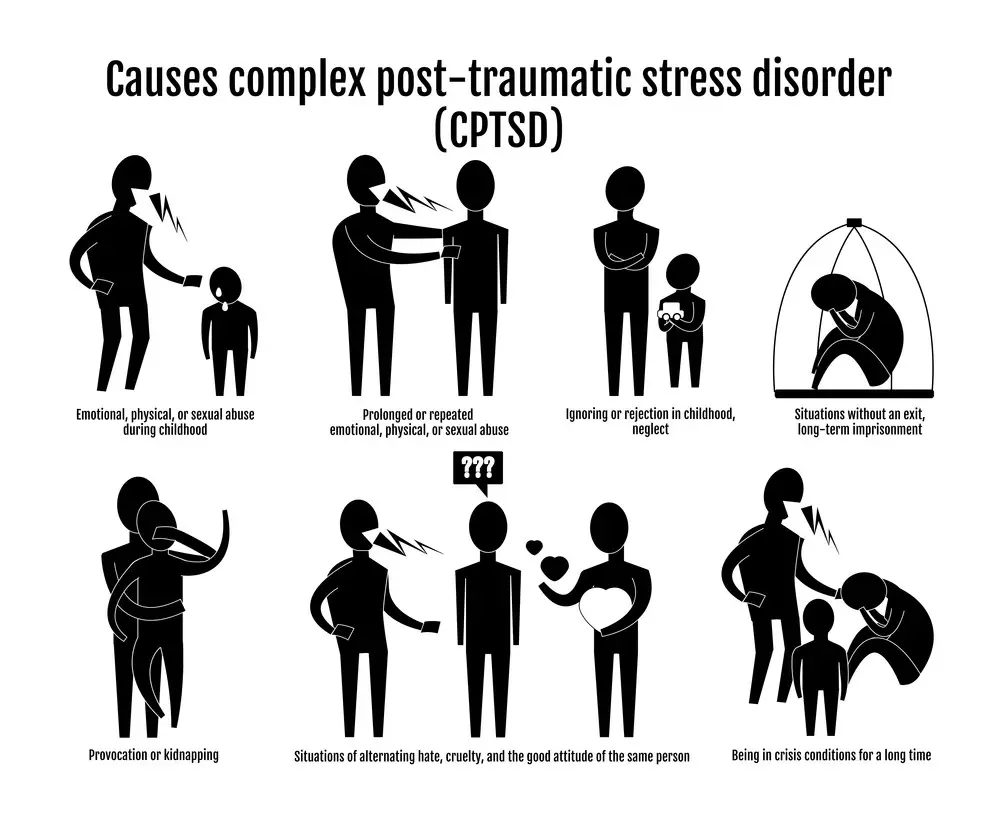
Exploring Complex PTSD: A Layer Deeper
Complex Post-Traumatic Stress Disorder (C-PTSD) is akin to PTSD. Still, it often stems from prolonged exposure to traumatic events or abuse, typically over a significant period, often in childhood or early adulthood. The impact goes deeper, often intertwining with one’s identity and relationships. Here’s a bit more on C-PTSD:
- Origin of Trauma:
- C-PTSD often originates from enduring complex trauma such as long-term child abuse, domestic violence, or being a prisoner of war, where the individual has little to no chance of escape.
- Characteristic Symptoms:
- Beyond the common symptoms shared with PTSD, individuals with C-PTSD may also experience difficulties regulating emotions, a sense of disconnection or detachment from oneself, and problems sustaining relationships.
- Treatment Pathways:
- Treatment may involve a combination of psychotherapy, cognitive behavioral therapy, dialectical behavior therapy, and eye movement desensitization and reprocessing (EMDR), often tailored to address the unique facets of complex trauma.
- Healing Journey:
- Healing from C-PTSD is a gradual process. Building a therapeutic alliance with a skilled therapist and fostering safe, supportive relationships are often integral to the healing journey.
- Long-Term Implications:
- With the right support and treatment, individuals can work through the layers of trauma, develop coping strategies, and build meaningful relationships.
Understanding C-PTSD is akin to peeling layers of an onion; each layer may bring tears but also brings you closer to the core, aiding in the healing process. Through comprehensive treatment and a supportive network, reclaiming one’s life from the grasp of complex trauma is within reach.
Treatment and Coping Strategies
Individuals with ASD and PTSD necessitate efficacious treatment and coping mechanisms to foster recovery and enhance life quality. Considering the sensitive nature of these disorders, expert treatment from seasoned, certified mental health professionals specializing in traumatic and complex symptoms is indispensable.
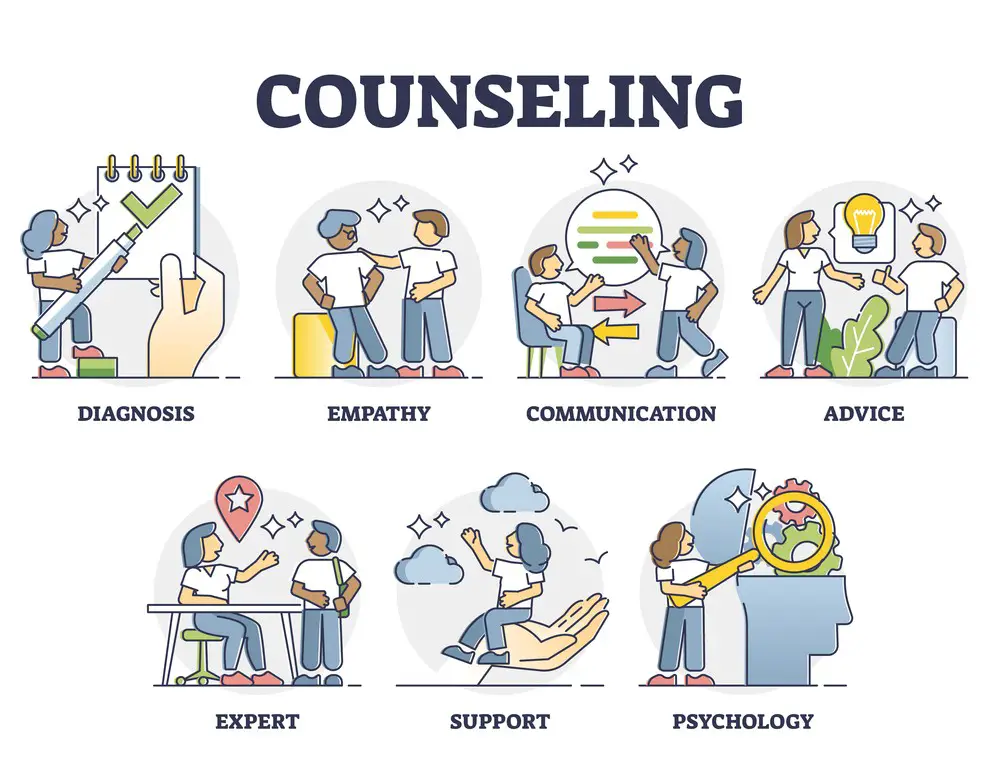
ASD Treatment
ASD treatment may encompass immediate interventions, therapeutic methodologies like cognitive-behavioral therapy, and a concentration on recovery anticipations to hinder PTSD evolution. Immediate interventions for ASD treatment may include providing emotional support, safety planning, and crisis management to ensure optimal outcomes.
Therapeutic approaches for ASD may include cognitive-behavioral therapy, psychotherapy, and trauma-focused therapy. The anticipated outcomes of ASD treatment may include educating the individual on their diagnosis, providing coping strategies, and fostering resilience.
PTSD Management
Managing PTSD entails investigating psychotherapy alternatives, comprehending the function of medications, and acquiring coping tactics to assist individuals in reclaiming control over their lives and emotions. Cognitive Behavioral Therapy (CBT), Eye Movement Desensitization and Reprocessing (EMDR), Prolonged Exposure Therapy (PE), and Acceptance and Commitment Therapy (ACT) are some of the most commonly used psychotherapeutic interventions for managing PTSD.
Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are the most commonly utilized medications for PTSD. Coping strategies such as relaxation techniques, mindfulness, and journaling can be utilized to help manage symptoms of PTSD.
 Discerning the Need for Therapy: Signs to Watch For
Discerning the Need for Therapy: Signs to Watch For
Recognizing when professional help is necessary can be a pivotal step toward healing for individuals dealing with ASD, PTSD, or C-PTSD. Here are some signs that indicate therapy may be essential:
- Persistent Distress: If symptoms cause significant distress or interfere with personal, social, or occupational functioning.
- Escalation of Symptoms: When symptoms intensify over time or new symptoms emerge.
- Avoidance Behavior: A pattern of avoiding reminders of the trauma or discussing the events.
- Detachment: Feeling detached from others, emotionally numb, or lacking positive emotions.
- Recurrent Intrusive Thoughts: Persistent flashbacks, nightmares, or intrusive thoughts about the traumatic event(s).
Mapping the Path to Healing: Setting Goals
Therapy is a collaborative endeavor. Setting clear, achievable goals can provide direction and motivation throughout the therapeutic journey:
- Short-Term Goals: Initially, goals may include reducing the frequency and intensity of flashbacks or improving sleep quality.
- Long-Term Goals: Over time, goals might evolve to improving interpersonal relationships, developing healthier coping strategies, or engaging in activities that were once avoided.
Celebrating Milestones: Recognizing Progress
Acknowledging progress, however small, can be a source of motivation and reassurance:
- Journaling: Keeping a journal can help track changes in symptoms, mood, and behavior over time.
- Therapist Feedback: Regular feedback from your therapist can provide an objective perspective on your progress.
- Reflect on Achievements: Take time to reflect on the achievements, be it better management of symptoms, improved relationships, or engaging in previously challenging activities.
Healing from ASD, PTSD, or C-PTSD is a journey that requires patience, support, and the right therapeutic guidance. Individuals can navigate the path toward recovery and improved quality of life by recognizing the need for professional help, setting clear goals, and acknowledging progress.
Conclusion
Understanding the critical differences between Acute and Post-Traumatic Stress Disorder is crucial for proper diagnosis, treatment, and management. By being aware of the causes, symptoms, and treatment options for both disorders, individuals and their loved ones can seek the help they need to overcome the challenges posed by these mental health conditions and lead fulfilling lives.
Frequently Asked Questions (FAQs)
What is the primary difference between Acute Stress Disorder and PTSD?
The primary difference between Acute Stress Disorder (ASD) and Post-Traumatic Stress Disorder (PTSD) is the duration of symptoms and when they occur. In ASD, symptoms typically emerge shortly after a traumatic event and last for at least three days but not longer than four weeks. On the other hand, PTSD involves persistent symptoms that last for over a month and can surface long after the traumatic experience, significantly affecting one’s daily life and functioning.
How long does it typically take for ASD to develop into PTSD?
The transition from Acute Stress Disorder (ASD) to Post-Traumatic Stress Disorder (PTSD) is unique for each individual and doesn’t have a fixed timeframe. Some people may recover from ASD within a few weeks or months, while others may develop PTSD after several months or even years. It largely depends on the nature of the trauma, individual resilience, and the presence of adequate support and coping mechanisms.
Can I manage ASD or PTSD on my own, or should I seek professional help?
Managing ASD (Acute Stress Disorder) and PTSD (Post-Traumatic Stress Disorder) can be challenging, and it often depends on the severity of your symptoms and individual circumstances. While some people may find relief and coping strategies through self-help techniques, many benefit greatly from seeking professional help, such as therapy, counseling, or medication, depending on the condition.
Evaluating your specific needs is essential, but reaching out to a healthcare provider or therapist is usually prudent, as they can provide tailored guidance and support to navigate these complex conditions.
- Left Arm Pain and Anxiety: Understanding the Relationship - November 23, 2023
- Anxiety Paralysis: Coping with Overwhelming Stress - November 23, 2023
- Anxious vs. Nervous: Differentiating Emotions and Responses - November 15, 2023
This site contains affiliate links to products. We will receive a commission for purchases made through these links.




 Discerning the Need for Therapy: Signs to Watch For
Discerning the Need for Therapy: Signs to Watch For
