As a BetterHelp affiliate, we receive compensation from BetterHelp if you purchase products or services through the links provided
Narcolepsy and sleep apnea are two distinct sleep disorders that affect millions of people worldwide. Both conditions can significantly impact a person’s quality of life and overall health, but they manifest differently and require unique approaches to diagnosis and treatment.
Narcolepsy is a neurological disorder that causes overwhelming daytime drowsiness and sudden sleep attacks. People with narcolepsy often struggle to stay awake for extended periods, regardless of their environment or activities. On the other hand, sleep apnea is a potentially serious condition characterized by paused or shallow breathing during sleep, which can lead to disrupted and poor-quality sleep.
In this article, we will explore the similarities, differences, and diagnostic criteria for narcolepsy and sleep apnea and the most effective treatment methods for each disorder. Understanding the distinctions and similarities between these two conditions can help affected individuals and their healthcare providers work together to develop targeted and personalized treatment plans.
Understanding Narcolepsy and Sleep Apnea
Narcolepsy
Narcolepsy is a neurological sleep disorder characterized by excessive daytime sleepiness, sudden and irresistible episodes of sleep, and a disturbed sleep-wake cycle. It affects about 1 in 2,000 people and is often underdiagnosed due to its subtle and varied symptoms. People with narcolepsy might also experience cataplexy, a sudden loss of muscle tone often triggered by strong emotions like laughter or surprise.
Narcolepsy has been linked to a deficiency in the neurotransmitter hypocretin, which is crucial in regulating the sleep-wake cycle. Treatment options for narcolepsy include stimulant medications to manage excessive daytime sleepiness and lifestyle adjustments like establishing regular sleep schedules and taking scheduled naps during the day.
Sleep Apnea

Sleep apnea is a sleep disorder involving the partial or complete blockage of the upper airway during sleep, leading to interrupted breathing and frequent awakenings. This fragmented sleep can cause excessive daytime sleepiness, snoring, and other health complications. Sleep apnea can be classified into three types:
- Obstructive sleep apnea (OSA): The most common form, caused by the collapse of soft tissues at the back of the throat, narrowing the airway.
- Central sleep apnea (CSA): A less common form, resulting from the brain failing to send proper signals to the muscles that control breathing.
- Complex sleep apnea syndrome: A combination of both obstructive and central sleep apneas.
Treatment options for sleep apnea include:
- Continuous positive airway pressure (CPAP) therapy: Using a machine that delivers continuous air pressure to keep the airway open during sleep.
- Lifestyle changes: Weight loss, avoiding alcohol and sedatives, and changing sleep positions can help improve symptoms in some cases.
- Oral appliances: Specially designed mouthpieces to reposition the jaw and tongue during sleep.
- Surgery: In severe cases, surgical procedures might be recommended to remove excess tissue or reposition the airway.
In conclusion, narcolepsy and sleep apnea are sleep disorders that can significantly impact an individual’s health and quality of life. Understanding their symptoms, causes, and available treatments is crucial for ensuring appropriate care and support for those affected by these conditions.
Types of Sleep Disorders and Apnea
Obstructive Sleep Apnea
Obstructive Sleep Apnea (OSA) is the most common type of sleep apnea. It occurs when the muscles in the throat relax, causing a partial or complete airway blockage during sleep. Individuals with OSA experience pauses in breathing, often followed by choking or gasping for air. Risk factors for OSA include obesity, smoking, alcohol consumption, and a family history of sleep apnea.
Central Sleep Apnea
Central Sleep Apnea (CSA) is less common than OSA and occurs when the brain fails to signal the muscles responsible for breathing during sleep. This results in a temporary cessation of breathing, leading to disrupted sleep. CSA can be caused by various medical conditions such as heart failure, stroke, or opioid use.
Complex Sleep Apnea
Complex Sleep Apnea Syndrome (CompSAS) is a combination of both OSA and CSA. It is usually diagnosed when an individual’s sleep apnea does not improve with a continuous positive airway pressure (CPAP) device, which is the standard treatment for OSA. In these cases, other treatments, such as adaptive servo-ventilation (ASV) may be recommended.
Type 1 Narcolepsy
Type 1 Narcolepsy is a neurological sleep disorder characterized by excessive daytime sleepiness, sudden loss of muscle tone (cataplexy), sleep paralysis, and hallucinations. It is caused by the loss of hypocretin-producing neurons in the brain, which is believed to be due to an autoimmune response. Genetic factors may also play a role in developing Type 1 Narcolepsy.
Type 2 Narcolepsy
Type 2 Narcolepsy shares the symptom of excessive daytime sleepiness with Type 1, but does not involve cataplexy. The cause of Type 2 Narcolepsy is poorly understood, but it is thought to involve dysfunction in the brain’s sleep-wake cycle. Both Type 1 and Type 2 Narcolepsy can be diagnosed through sleep studies and medical evaluations, and they are often treated with medications to manage symptoms, such as stimulants and antidepressants.
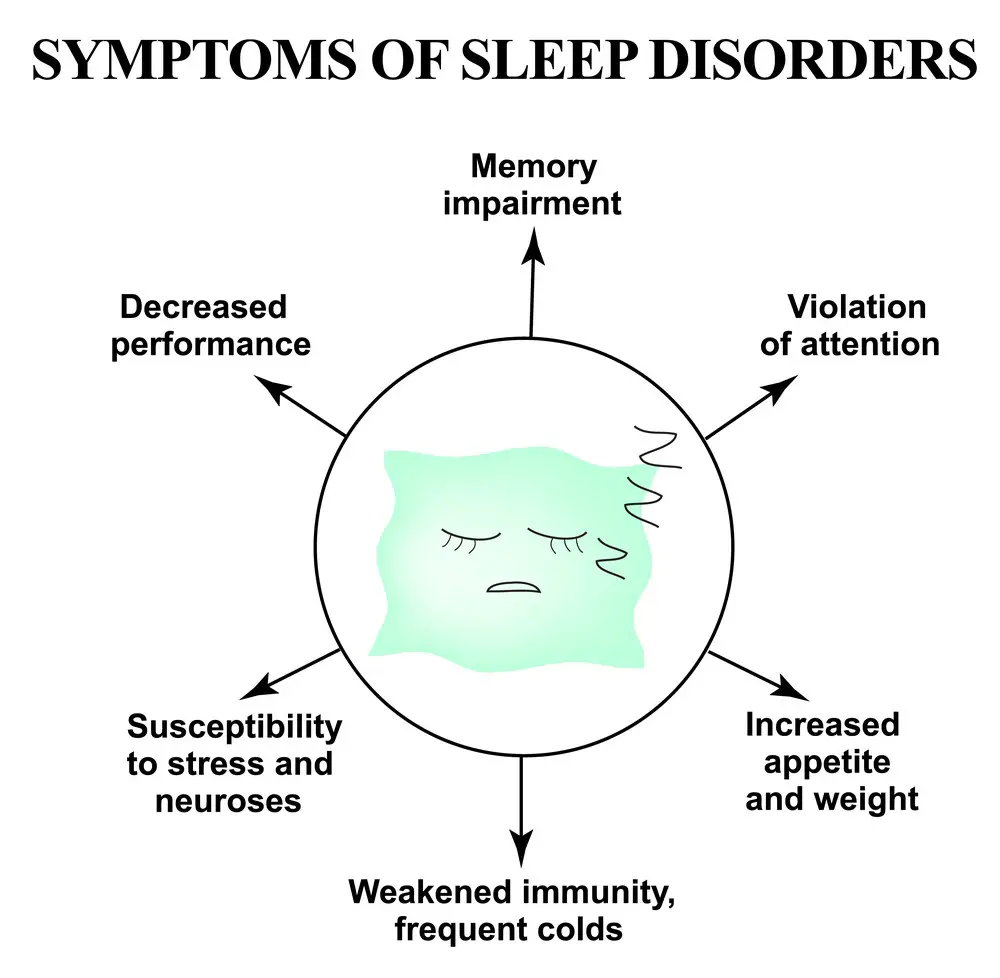
Common Symptoms
Narcolepsy and sleep apnea are sleep disorders that can significantly impact a person’s daily life. Though they share some common symptoms, they also have unique characteristics that differentiate them.
Narcolepsy Symptoms
The following symptoms characterize narcolepsy:
- Excessive daytime sleepiness: People with narcolepsy often experience an overwhelming urge to sleep during the day, which can interfere with daily activities.
- Sleep attacks: These are sudden, involuntary episodes of sleep that can occur at any time, even during activities such as talking or eating.
- Sleep paralysis: This is a temporary inability to move that can occur while falling asleep or waking up from sleep.
- Hallucinations: They can occur during the transition between wakefulness and sleep and may involve vivid, dream-like experiences.
- Loss of muscle tone: In some cases, narcolepsy can cause a sudden loss of muscle strength, known as cataplexy, in response to strong emotions like laughter, anger, or excitement.
Sleep Apnea Symptoms
On the other hand, sleep apnea presents with the following symptoms:
- Loud snoring: This is a prominent symptom of sleep apnea, and it can be disruptive for the person affected and those around them.
- Breathing pauses: People with sleep apnea experience intermittent pauses in breathing due to airway obstruction, which disrupts their sleep.
- Daytime sleepiness: Similar to narcolepsy, individuals with sleep apnea may have difficulty staying awake during the day due to sleep disruptions at night.
- Morning headaches: Sleep apnea can lead to frequent headaches upon waking, often due to a lack of oxygen during sleep.
- Dry mouth: This can occur in sleep apnea patients as they may breathe through their mouths during sleep to compensate for the obstruction in their airways.
- Vivid dreams: Sleep disruptions from sleep apnea can cause vivid or frequent dreaming, often related to awakening during REM sleep stages.
Both narcolepsy and sleep apnea share symptoms such as daytime sleepiness and sleep disruptions. However, the unique symptoms, including sleep attacks, sleep paralysis in narcolepsy, and loud snoring and breathing pauses in sleep apnea, help differentiate these two sleep disorders.
Diagnosis and Testing
Polysomnography
Polysomnography, a sleep study, is a common test used in diagnosing narcolepsy and sleep apnea. It involves monitoring brain waves, eye movements, heart rate, and muscle activity while the patient sleeps. This allows doctors to evaluate sleep patterns and identify abnormalities contributing to excessive daytime sleepiness or unwanted sleep events.
For sleep apnea, the test helps detect interruptions in breathing or significant reductions in airflow during sleep. In the case of narcolepsy, polysomnography helps identify rapid eye movement (REM) sleep-related issues, such as a shorter than normal REM latency.
Multiple Sleep Latency Test
The Multiple Sleep Latency Test (MSLT) is another diagnostic tool primarily used to identify narcolepsy. It measures the time it takes for a person to fall asleep during a series of daytime naps under controlled conditions. An individual with narcolepsy typically falls asleep more quickly and enters REM sleep more rapidly than someone without the condition. In some cases, the MSLT might also be used to assess the severity of sleep apnea.
Lumbar Puncture
For a more definitive diagnosis of narcolepsy, a lumbar puncture, or spinal tap, may be performed. This test involves collecting a sample of cerebrospinal fluid (CSF) from the lower back. Researchers have found that individuals with narcolepsy often have low levels of the brain chemical hypocretin, which helps regulate sleep and wakefulness. By analyzing the CSF sample, doctors can confirm a narcolepsy diagnosis if hypocretin levels are significantly reduced.
While lumbar puncture is not commonly used in diagnosing sleep apnea, it may be performed if concerns about other neurological causes for sleep disturbances need to be ruled out.
Risk Factors and Causes
Narcolepsy and sleep apnea have different risk factors and causes, though some factors can contribute to both conditions.
A deficiency of the neurotransmitter hypocretin primarily causes narcolepsy. This deficiency is often due to an autoimmune response, where the body mistakenly attacks the cells that produce this neurotransmitter. Common risk factors for narcolepsy include:
- Cataplexy: A sudden loss of muscle tone, often triggered by emotions. This is more common in individuals with narcolepsy type 1.
- Family history: Though rare, genetics can play a role in developing narcolepsy. Those with a family history of the condition have a slightly higher risk.
Sleep apnea, on the other hand, has different causes and risk factors. Obstructive sleep apnea, the most common form, results from a physical airway blockage during sleep. Central sleep apnea occurs when the brain fails to signal the muscles to breathe. Risk factors for sleep apnea include:
- Obesity: Excess body weight, particularly around the neck, can contribute to the obstruction or collapse of the airway during sleep.
- Aging: The risk of sleep apnea increases as muscle tone decreases and tissues become more prone to collapse.
- Family history: Genetic factors can also contribute to an increased risk of sleep apnea.
- Hypothyroidism: An underactive thyroid can lead to weight gain and a narrowed airway, increasing the risk of sleep apnea.
- Tonsils: Enlarged tonsils can obstruct the airway, particularly in children, leading to sleep apnea.
- Overweight: Like obesity, being overweight can cause excess tissue around the airway, increasing the likelihood of sleep apnea.
Addressing these risk factors, such as maintaining a healthy weight and managing underlying medical conditions, can help reduce the likelihood of developing narcolepsy or sleep apnea.
Treatment Options and Lifestyle Changes
Medications
In treating narcolepsy, medications such as stimulants and antidepressants may be prescribed. Stimulants, like modafinil, help patients with excessive daytime sleepiness by promoting wakefulness. Antidepressants, on the other hand, can help manage cataplexy and other symptoms related to REM sleep disruptions.
For sleep apnea treatment, medications are less commonly used. However, in some cases, doctors may prescribe medication to address underlying health conditions, reducing the severity of sleep apnea symptoms.
Continuous Positive Airway Pressure (CPAP)

Continuous Positive Airway Pressure (CPAP) therapy is a common treatment for obstructive sleep apnea. Patients wear a mask that covers the nose and mouth, connected to a machine that delivers pressurized air. This air pressure helps keep the airway open, preventing the collapse that causes apneas.
Oral Devices and Mouthpieces
Oral devices and mouthpieces can also treat sleep apnea, particularly for mild to moderate cases. These devices work by repositioning the jaw and tongue, helping to keep the airway open during sleep. They can be custom-fit to the patient for comfort and effectiveness.
Lifestyle Changes
For both narcolepsy and sleep apnea, making lifestyle changes is beneficial. Some recommended changes include:
- Maintaining a regular sleep schedule
- Adopting a healthy diet and exercise routine
- Avoiding caffeine, nicotine, and alcohol, especially close to bedtime
- Practicing good sleep hygiene, such as creating a comfortable sleep environment and establishing a bedtime routine
In some cases, treating underlying health conditions or losing weight may also help alleviate the severity of narcolepsy and sleep apnea symptoms. Patients must work closely with their healthcare providers to assess the most suitable treatment options for their needs.
Sleep-Wake Cycle and REM Sleep
The sleep-wake cycle is essential to human health, regulating various bodily functions and ensuring proper rest. This cycle consists of two primary states: non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep.
The body undergoes physical restoration during NREM sleep, and brain activity is relatively low. In contrast, REM sleep is characterized by more active brain function, including vivid dreaming. A healthy sleep-wake cycle consists of several cycles of NREM and REM sleep, with REM sleep typically occurring every 90 minutes.
Both narcolepsy and sleep apnea can disrupt the sleep-wake cycle, leading to sleep deprivation and impaired quality of life. In individuals with narcolepsy, the primary issue is a deficiency in the neurotransmitter hypocretin, which affects sleep and wakefulness regulation. This deficiency can result in:
- Fragmented sleep, with frequent awakenings
- Intrusions of REM sleep into wakefulness
- Scheduled naps to combat excessive daytime sleepiness
On the other hand, sleep apnea is characterized by a partial or complete blockage of the airways during sleep, leading to interrupted breathing and frequent awakenings. Notably, sleep apnea does not typically affect REM sleep duration; however, it can lead to:
- Fragmented sleep, with reduced sleep efficiency
- Decreased REM sleep latency, or the time it takes to enter REM sleep after falling asleep
- Sleep deprivation due to continuous breathing interruptions
In conclusion, narcolepsy and sleep apnea can negatively impact the sleep-wake cycle and REM sleep. While the underlying causes and specific sleep disruptions differ, it is essential for individuals experiencing sleep issues to seek medical advice to address these concerns and improve their overall sleep quality.
Mental Health and Emotional Aspects
Narcolepsy and sleep apnea are both sleep disorders that can significantly impact an individual’s mental health and emotional well-being. People with these conditions often experience various difficulties affecting their mood, self-esteem, and relationships.
One common issue for individuals with narcolepsy is the experience of hypnagogic hallucinations. These vivid, often disturbing, dream-like experiences can occur between waking and falling asleep. This can lead to confusion, fear, and anxiety for the person experiencing them.
Depression is another common concern among people with both narcolepsy and sleep apnea. The chronic fatigue and disrupted sleep patterns associated with these conditions can contribute to a persistent low mood. This, in turn, can exacerbate other symptoms, creating a vicious cycle for the sufferer.
In addition to depression, individuals with these sleep disorders may also struggle with:
- Low libido: Sleep disturbances can negatively impact a person’s sex drive, leading to frustration and strained relationships.
- Emotional outbursts: Sudden, uncontrollable laughter or crying, known as cataplexy, can be a symptom of narcolepsy. This can be both embarrassing and distressing for the individual.
- Mood swings: The chronic lack of quality sleep may lead to irritability and emotional instability.
It’s important to note that the emotional toll of living with a sleep disorder can be just as significant as the physical symptoms. Therefore, comprehensive treatment plans should address both the mental health and emotional aspects of these conditions. Therapy, counseling, and support groups can be valuable resources for individuals navigating the challenges of narcolepsy and sleep apnea.
Coexisting Conditions and Related Disorders
Narcolepsy and sleep apnea are distinct sleep disorders, but they can coexist with other conditions and related disorders. Identifying and addressing these accompanying issues is essential to provide comprehensive care for patients with multiple sleep problems.
Insomnia, for instance, is a common issue affecting narcolepsy and sleep apnea patients. It hinders the ability to fall or stay asleep, causing the affected individual further sleep deprivation and aggravating their sleep disorders.
Headaches can also arise due to inadequate sleep experienced by individuals with narcolepsy or sleep apnea. Chronic sleep deprivation and fragmented sleep may contribute to tension-type headaches or even migraines, affecting the quality of life of the affected person.
Many patients with narcolepsy or sleep apnea take medications such as antihistamines and beta-blockers for their treatment. Antihistamines are often used to alleviate allergy symptoms, but they can exacerbate sleepiness in narcolepsy patients. Meanwhile, beta-blockers, prescribed for heart conditions and high blood pressure, can sometimes negatively impact sleep patterns and cause nightmares, further complicating sleep apnea management.
Neurological disorders, such as Parkinson’s disease and multiple sclerosis (MS), can also present comorbidities with narcolepsy and sleep apnea. Both Parkinson’s disease and MS can disrupt normal sleep patterns and worsen symptoms of existing sleep disorders. In the case of Parkinson’s disease, patients may experience increased sleep fragmentation, restless leg syndrome, and REM sleep behavior disorder. For those with multiple sclerosis, there can be an increased prevalence of sleep apnea, exacerbating fatigue and cognitive function issues experienced by MS patients.
In conclusion, addressing the complexities of coexisting conditions and related disorders in patients with narcolepsy and sleep apnea is crucial for improving their overall well-being and quality of life. Evidence-based treatment strategies and a multidisciplinary approach are vital in managing these challenging circumstances.
FAQs
What is the difference between narcolepsy and sleep apnea?
Narcolepsy is a neurological disorder in which an individual experiences excessive daytime sleepiness and sudden episodes of sleep during the day. Sleep apnea is a sleep disorder in which an individual’s breathing repeatedly stops and starts during sleep, causing disruptive and restless sleep.
What are the common symptoms of narcolepsy and sleep apnea?
Narcolepsy:
- Excessive daytime sleepiness
- Cataplexy (sudden loss of muscle tone)
- Sleep paralysis
- Hypnagogic hallucinations
Sleep Apnea:
- Snoring
- Gasping for air during sleep
- Morning headaches
- Daytime fatigue
What causes narcolepsy and sleep apnea?
The exact cause of narcolepsy is unknown, but it is believed to be related to abnormalities in the brain chemicals that regulate sleep and wake cycles, specifically the lack of the neurotransmitter hypocretin. Sleep apnea, however, can be caused by various factors such as obesity, family history, smoking, nasal congestion, or alcohol consumption.
How are narcolepsy and sleep apnea diagnosed and treated?
Diagnosis:
Narcolepsy is typically diagnosed through a thorough clinical examination, sleep history, and sleep studies such as polysomnography (PSG) and multiple sleep latency test (MSLT). Sleep apnea can be diagnosed with a sleep study, primarily through overnight polysomnography.
Treatment:
For narcolepsy, treatment options include prescribed medications like stimulants, antidepressants, and sodium oxybate to help manage the symptoms. Sleep hygiene, scheduled naps, and support from a mental health professional may also be beneficial.
Sleep apnea can be treated with lifestyle changes like losing weight or quitting smoking. More severe cases might require continuous positive airway pressure (CPAP) therapy or other oral devices to maintain an open airway during sleep. Surgery may sometimes be recommended to remove excess tissue in the airway.
- 7 Ideas to Help You Relax and Unwind on a Family Vacation - April 27, 2025
- How Having Cybersecurity Protection Helps You Relax - April 25, 2025
- 8 Reasons Why Spending Time Outside Calms You Down - April 25, 2025
This site contains affiliate links to products. We will receive a commission for purchases made through these links.