As a BetterHelp affiliate, we receive compensation from BetterHelp if you purchase products or services through the links provided
Dealing with a prolapsed bladder can be both physically and emotionally challenging. One of the most common concerns for individuals facing this condition is how to sleep comfortably at night. This article will discuss helpful strategies for sleeping with a prolapsed bladder, ensuring you get the rest you need while contributing to your overall health and well-being.
A prolapsed bladder can cause discomfort and disrupt your daily life, including your ability to enjoy a restful night’s sleep. As sleep is essential for overall health and mental well-being, addressing the impact a prolapsed bladder may have on your sleep quality is essential. Treatment options vary based on the severity of the prolapse, but lifestyle changes, exercises, and medical interventions can all help provide relief during this challenging time.
Key Takeaways
- Strategies for sleeping with a prolapsed bladder can improve your nighttime comfort.
- Sleeping challenges may arise due to discomfort from prolapsed bladder, but treatment options are available.
- Making lifestyle changes and obtaining medical help can enhance sleep quality for individuals with prolapsed bladders.
Understanding Prolapsed Bladder

Identifying the Problem
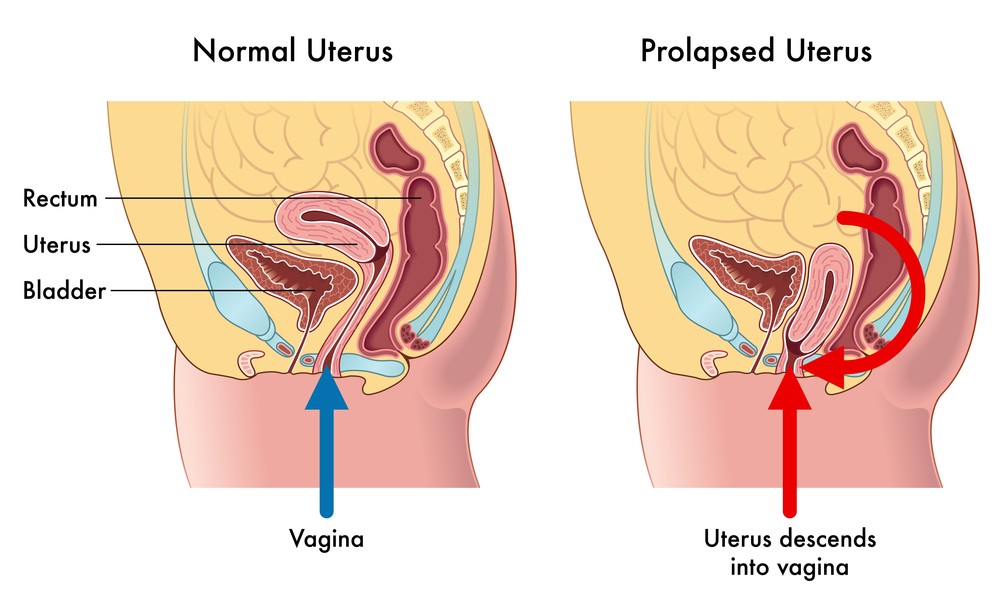
A prolapsed bladder, also known as a cystocele or fallen bladder, is a condition where the bladder falls into the vaginal canal. This happens when the pelvic floor muscles and tissues weaken or stretch, affecting their ability to support the pelvic organs properly.
Typically, the problem is more common among women due to factors like age, childbirth, menopause, pregnancy, and obesity. Identifying this issue early and consulting with a doctor is essential, as neglecting it can result in further complications.
Causes and Risk Factors
Several factors increase the risk of prolapsed bladder:
- Age: As you age and reach menopause, the risk increases due to the natural reduction of estrogen levels.
- Childbirth: Vaginal deliveries can cause damage to the pelvic muscles.
- Pregnancy: Carrying a baby puts extra pressure on the pelvic floor.
- Obesity: Being overweight adds additional strain on the pelvic floor muscles.
- Heavy lifting, coughing, and straining: These activities increase intra-abdominal pressure and can lead to weakened pelvic support.
Understanding these risk factors can help you be proactive about prevention and management strategies.
Common Symptoms
You may experience the following symptoms with a prolapsed bladder:
- Discomfort or pain in the pelvic area
- A bulge or feeling of heaviness in the vagina
- Urinary incontinence (trouble controlling urine flow)
- Nocturia (the need to urinate frequently at night)
- Urgent or frequent urge to urinate
- Leakage of urine during activities like coughing or sneezing
Pay attention to these symptoms and consult your doctor if they occur.
Dealing with Diagnosis
Your doctor can diagnose a prolapsed bladder through:
- Pelvic exam: A physical examination to check for visible signs of prolapse.
- Ultrasound: Imaging the pelvic region to assess the severity of the prolapse.
- MRI: More detailed imaging may be ordered to understand the issue better.
Though dealing with the diagnosis may be challenging, it’s crucial to address the issue and work with your healthcare professional to find the best treatment plan for you. Remember that early intervention can lead to better outcomes.
Impact on Sleep and Quality of Life
Sleep Quality Concerns
A prolapsed bladder can lead to various sleep quality concerns. When you don’t feel comfortable, it isn’t easy to achieve restful sleep. The pressure and heaviness that come with a prolapsed bladder may cause you to wake up frequently throughout the night, leading to sleep disturbances. Your well-being is also affected, as poor sleep can contribute to feelings of depression and anxiety.
To combat this, it’s essential to focus on good sleep hygiene. Some tips for better sleep include:
- Establishing a consistent sleep schedule
- Creating a relaxing pre-sleep routine
- Limiting exposure to screens and electronic devices before bedtime
- Ensuring your bedroom is calm, quiet, and dark
Key takeaway: Prioritize sleep hygiene to improve sleep quality and overall well-being.
Effect on Everyday Activities
A prolapsed bladder can also have a significant impact on your day-to-day life. As you go about your regular activities, you might feel a constant sense of fullness or discomfort, especially while standing for extended periods. This can affect your energy levels and overall mood.
Another area of concern is the increased urgency for bathroom movements. Frequent trips to the bathroom can disrupt your routines and become a source of anxiety in social situations.
To alleviate some of these issues, you can:
- Schedule regular bathroom breaks in your daily routine, even if you don’t feel the urge to go
- Perform pelvic floor exercises to strengthen the muscles and support the bladder
- Use over-the-counter bladder supports to reduce discomfort and pressure
Key takeaway: Managing the effects of a prolapsed bladder on everyday activities will help you maintain your quality of life and well-being.
Treatment Options for Prolapsed Bladder
Self-Care and Lifestyle Changes
If you have a prolapsed bladder, you can try several self-care and lifestyle changes to alleviate symptoms. These include:
- Pelvic floor exercises: Kegel exercises can help to strengthen the muscles supporting your bladder. Do these daily to improve your condition.
- Good bladder habits: Make a point of emptying your bladder when using the restroom.
- Avoiding caffeine and alcohol can irritate the bladder, so limiting or eliminating them from your diet is wise.
Key takeaway: Self-care and lifestyle changes can help manage a prolapsed bladder with minimal medical intervention.
Medical Treatments
For moderate prolapse, your healthcare provider may recommend medical treatments. These options include:
- Medication: Estrogen replacement therapy can help some individuals by strengthening the bladder’s supporting tissues.
- Pessary: This non-surgical device can be inserted into the vagina to help support the bladder.
It’s important to discuss these treatments with your doctor to determine the best course of action based on the severity of your condition.
Key takeaway: Medical treatments like estrogen replacement therapy or using a pessary can help manage moderate cases of prolapsed bladder.
Surgery Options
For severe prolapse, surgery may be the recommended treatment option. There are a variety of surgical procedures available, including:
- Reconstructive surgery: This procedure involves repairing the weakened pelvic floor muscles to support the bladder better.
- Hysterectomy: In some cases, removing the uterus may help alleviate the strain on the pelvic floor.
As with any surgery, there are risks and potential complications. Consult with your healthcare provider to discuss if surgery is the best option.
Key takeaway: Surgery may be needed to treat a prolapsed bladder in severe cases. Always consult with your healthcare provider to explore all your treatment options.
Sleeping with a Prolapsed Bladder
Adopting Comfortable Sleep Positions
To sleep comfortably with a prolapsed bladder, experimenting with different sleep positions can be helpful. Try side sleeping, as it can ease pressure on your pelvis and bladder. You can also consider elevating your hips with a pillow to reduce bladder discomfort.
- Side sleeping: This position can help alleviate pressure on your bladder, providing a more comfortable night’s rest.
- Using a wedge pillow: Placing a wedge pillow under your hips when side sleeping may help minimize discomfort and improve sleep quality.
Creating a Restful Sleep Environment
A conducive sleep environment plays a critical role in enhancing sleep quality. Consider making these changes to create a relaxed atmosphere for sleeping with a prolapsed bladder:
- Keep your bedroom calm, dark, and quiet for optimal comfort.
- Establish a consistent sleep schedule, going to bed and waking up at the same time daily.
- Limit caffeine intake several hours before bedtime, as it may irritate your bladder and disrupt sleep.
Dealing with Night-Time Symptoms
Nocturia (frequent nighttime urination) and urine leakage are common problems for people with a prolapsed bladder. Implementing healthy bladder habits can help reduce these symptoms:
- Use the bathroom before bedtime to minimize the need for nighttime visits.
- Manage fluid intake in the evening, ensuring not to drink excessively before bedtime.
- Keep a night light or flashlight close to the bed to locate the bathroom during nighttime visits quickly.
Key takeaway: Implement healthy bladder habits to cope with nocturia and urine leakage, common symptoms of a prolapsed bladder that can affect sleep quality.
Consulting Healthcare Professionals
Finally, don’t hesitate to consult your doctor or healthcare provider when dealing with a prolapsed bladder. They may have additional recommendations or treatment options to help you sleep comfortably:
- Discuss your symptoms and concerns with your healthcare provider.
- Explore potential treatments tailored to your specific needs.
- Follow your doctor’s guidance on necessary lifestyle changes and bladder-supporting exercises.
Remember, seeking professional advice is essential to manage your prolapsed bladder and improve overall sleep quality.
Frequently Asked Questions
What is the best sleeping position for a prolapsed bladder?
The best sleeping position for a prolapsed bladder alleviates pressure on the bladder and provides comfort. For many, this means sleeping on their side with a pillow between their knees. This position helps align the spine and pelvis, reducing strain on the pelvic organs. Experiment with different positions and pillows to find what works best for you.
Key takeaway: Side sleeping with a pillow between the knees can help relieve pressure and discomfort.
Does lying down worsen the condition?
Lying down can help alleviate some of the discomfort caused by a prolapsed bladder. When you lie down, gravity no longer pulls on your pelvic organs, which can reduce the feeling of pressure. However, be sure to find a comfortable position that doesn’t strain your bladder or other organs. Adjust pillows and blankets to help support your body.
Which sleeping positions put less pressure on the bladder?
Generally, side sleeping positions are best for reducing pressure on the bladder. This is especially true when using a pillow between your knees to align your spine and pelvis. Avoid sleeping on your stomach, which can increase bladder and pelvic organ pressure. Back sleeping may be okay for some people, but it is essential to ensure proper support for your lower back with a pillow.
Are there any activities to avoid with a prolapsed bladder?
Avoiding activities that worsen the condition or cause discomfort is essential with a prolapsed bladder. Some activities to avoid include:
- Heavy lifting
- Straining during bowel movements
- High-impact exercises like running or jumping
- Prolonged standing or sitting
Instead, focus on low-impact activities like walking, swimming, or gentle yoga to help maintain your fitness without aggravating your prolapse.
Is walking safe with a bladder prolapse?
Yes, walking is a safe and gentle exercise that can benefit people with a prolapsed bladder. Walking helps promote circulation and strengthen the pelvic floor muscles, alleviating symptoms and improving your overall condition. Start slowly and gradually build up the frequency and duration of your walks.
Key takeaway: Walking is a safe, gentle exercise for those with a prolapsed bladder.
Can a prolapsed bladder cause bloating?
A prolapsed bladder may cause feelings of fullness, discomfort, and even pressure in the lower abdomen, contributing to bloating. However, bloating can also be a symptom of other gastrointestinal issues unrelated to bladder prolapse. If you’re experiencing persistent bloating, it’s essential to consult your healthcare provider to determine the cause and receive appropriate treatment.
This site contains affiliate links to products. We will receive a commission for purchases made through these links.